Healthcare facilities are being continually dragged onto the battlefield, and patients and their doctors and nurses are sacrificed in the process. Since 2015, we have marked the loss of 26 MSF staff in 10 separate events, including during the storming or bombing of hospitals. Over the last five years, our staff have lost their lives in Ethiopia, Afghanistan, South Sudan, Syria, Yemen, and Central African Republic. In total, we have mourned the deaths of 97 colleagues, who have been killed in 59 separate events, the first recorded event occurring in 1989.
In the biggest single event, our trauma hospital in Kunduz, Afghanistan was destroyed in a US military airstrike in October 2015. Forty-two people were killed, including 14 of our staff. In Afghanistan’s capital, Kabul, in April 2020, armed groups stormed our maternity wing in Dasht-e-Barchi hospital, killing 16 women and an MSF midwife.
In Syria, hospitals and clinics we support have been routinely bombed. Ambulances in war-torn Yemen often come under attack. Armed incursions into our health facilities have occurred in places including Sudan.
Not only military attacks
But attacks on health care aren't limited to just the military. Medical workers and civilians are finding themselves caught up in indiscriminate violence by armed groups.
Many times in recent years, we have had to stop providing medical care and withdraw our teams in several countries because of raids at gunpoint in our hospitals. In December 2020, following a series of violent incidents against our teams, we made the difficult decision to end our activities in Fizi territory, northeastern Democratic Republic of Congo.
Sadly, some of our patients and staff have also been killed or injured. During 2017 in Central African Republic (CAR), people seeking shelter in our hospital in Batangafo from the inter-community violence were attacked by armed men. In another incident in CAR, a baby was shot dead in her mother's arms in front of our staff while seeking shelter in our hospital in Zemio.

Health facilities destroyed in CAR conflict
Armed men have stopped our ambulances in the street, threatened our staff at gunpoint, and pulled out the patient in back of the ambulance and taken them away, denying them medical care. In January 2021, a clearly-marked MSF ambulance transferring patients between Douentza and Sévaré, in central Mali, was violently stopped by armed men. The ambulance and its occupants – including patients, driver and medical staff – were detained for several hours; one of the patients died as a result.
UN Resolution 2286
It was the destruction of the Kunduz Trauma Centre, and the devastating assault on health facilities in Syria and Yemen, that led to UN Security Council (UNSC) Resolution 2286 being passed in May 2016.
MSF worked hard to advocate for states to ensure that the provision of medical care on both sides of the frontline is protected. The resolution was necessary. It was a political reassertion of the legitimacy and protected status of humanitarian medical action, at a time when medical care was under deadly aerial attack from states, including member states of the UNSC or coalitions they backed.
The resolution also enhanced the protection of health care in conflict. It formally extended protection under International Humanitarian Law (IHL) to humanitarian and medical personnel exclusively engaged in medical duties. This includes staff, medical activities and facilities of private humanitarian organisations, such as MSF. It also clarified and solidified the protection of hospitals.

Five years on, medical care is still being attacked.
However, the reality is that in the five years since the resolution was passed, little has changed for those on the ground in conflict zones. Hospitals and medical and humanitarian workers continue to be threatened and targeted in conflict. The adoption of the resolution has not solved the problems encountered by our teams on the ground.
Practically speaking, the resolution has done little to protect those for whom its adoption was designed to protect.
States must clarify and reassert their commitment to protect the wounded and sick, and those treating them, as humanitarian and medical aid face a growing trend of criminalisation.

How can we operate?
We accept that operating in war zones and conflict settings is not without its risks. But there are measures we take to help reduce the risk of being attacked by parties in a conflict.
Medical ethics and negotiation
Under medical ethics, the denial of lifesaving aid is non-negotiable. Patients brought into our hospital emergency rooms should be treated, regardless of who they are, or what side of the frontline they’re on or happen to live.
This view is unfortunately not shared by all, and we are working to counter the ‘criminalisation’ of medical care on the battlefield. On the one hand, under many domestic counter-terrorism laws, any aid provided to areas where so-called “terrorists” operate is grounds for prosecution and those areas are typically very hard to access.
But on the other hand, where we are able to reach difficult areas (and some areas that aren’t difficult to reach), armed groups attack, abduct and kill humanitarian and medical workers.
While the threat to medical humanitarian organisations is double and different in nature, the root of why we try to access these areas is the same – to provide much-needed medical care to people. To that end, we engage all parties to the conflict to enable us to provide medical care in war and conflict zones safely. We re-affirm to all sides that our only objective is to provide care to people and to not interfere with any political or military agenda.

We also employ mechanisms such as ensuring we’re clearly identified, and that groups know who and where we are. In places like Yemen and Afghanistan, our logo is very clearly marked on our ambulances and on the roof of our hospitals, and we proactively share the coordinates of our medical structures. These negotiations and mechanisms require constant maintenance and vigilance through dialogue with parties to the conflict.
It's crucial for us and the work we do that we preserve the sanctity and protection of medical care, and that we have access to all parties in a conflict to secure that protection. Establishing these ‘deconfliction’ arrangements – which then must be respected by all sides – is crucial to prevent attacks.
States must take all the necessary steps to ensure the maximum protection for the wounded and the sick, and medical and humanitarian personnel.

Dealing with the aftermath of attacks
Nonetheless, attacks on healthcare and medical workers continue to happen. After an attack, it’s critical for us to establish the facts on what happened and why, and to establish whether we can put teams back on the ground. We ask, “what happened?”; “how can we prevent a future attack?” “Can we maintain a team in a specific context?”
Where the attack was believed to be carried out by local or non-state armed groups, there is often very few possible legal means – such as through the courts or formal investigation channels – to find answers or deliver justice. Our teams try to engage with local leaders or these groups directly. We ask them for the reasons behind the attack and assess whether we can continue operating in that context. We also emphasise our neutrality and our role to provide humanitarian assistance and medical care to all people.
In the wake of an attack where military or a state armed group was involved, an independent and impartial fact-finding investigation can often be an effective way to bring accountability and help put in place measures to avoid it happening again. After the attack which destroyed our hospital in Kunduz, Afghanistan, we asked the International Humanitarian Fact-Finding Commission to establish the facts of this event.
Created in 1991 under the Geneva Conventions that govern the rules of war, the IHFCC – which is not a UN body – has been set up precisely to independently investigate violations of humanitarian law. However, the United States refused to cooperate with an independent investigation on Kunduz, despite our intense lobbying.
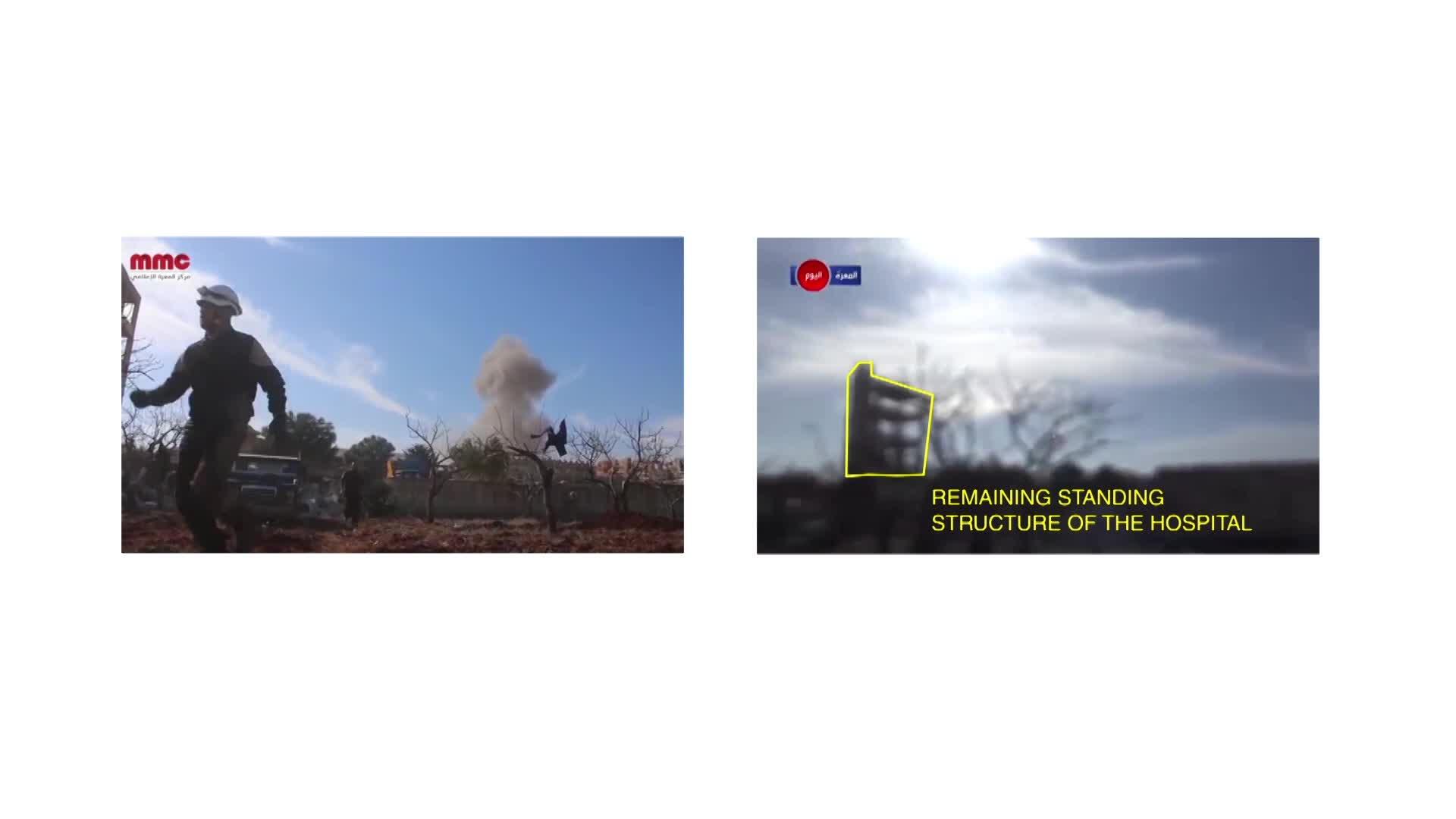
Using technology to establish the facts behind hospital bombings
Nonetheless, investigations need to happen to try to establish accountability and bring some form of justice to the casualties – ideally without the suspected perpetrators being also part of, or allied to, the judge and jury. Three years after the 2016 bombing of the MSF-supported Shiara Hospital in northern Yemen, the UK and US-supported Joint Incidents Assessment Team – which was appointed by the Saudi and Emirati-led Coalition engaged in Yemen – failed to provide any true accountability.
Following incidents like these, MSF conducts our own internal review and assessment of the event, often making our own findings public. But sometimes – regardless of whether the circumstances were clear or not – we decide it’s simply too dangerous for our patients, our staff, or both, to continue working in a context where there has been an attack. On a number of occasions, this has led to the extremely difficult and heart-breaking decision to withdraw – the consequences of which often means people are left without adequate access to healthcare.
Following the attack on our maternity wing in Dasht-e-Barchi, we decided to leave, as the risk of future loss of life in attacks was considered too great. This left the women of western Kabul and surrounds – the majority from the marginalised Hazara community – without specialised maternity care, in a country where maternal and neo-natal mortality are high.



