Two days ahead of the G20 summit in Germany, Médecins Sans Frontières (MSF) and the Stop TB Partnership released the third edition of Out of Step, a report highlighting the need for governments to increase efforts to combat tuberculosis (TB).
The report reviews TB policies and practices in 29[1] countries – which account for 82 per cent of the global TB burden – and shows that countries can do much more to prevent, diagnose and treat people affected by TB. Although TB is preventable and treatable, it remains the world's deadliest infectious disease. In 2015 alone, 1.8 million people died from it, and the majority (54 per cent) of the 10.4 million people with TB lived in the countries represented at the G20 summit. Despite its deadly toll, most countries lag behind in implementing the new tools available to tackle TB. During the G20 summit, governments must include TB in their efforts to tackle the wider problem of drug-resistant infections.
“TB is an ancient killer, but we have the knowledge and the tools to tackle this disease; many countries are just not making use of these advances, and people are dying as a result,” said Lucica Ditiu, executive director of The Stop TB Partnership. “We’re calling on the G20 leaders to wake up and do something to stop the unnecessary deaths and the spread of TB, including drug-resistant TB.”
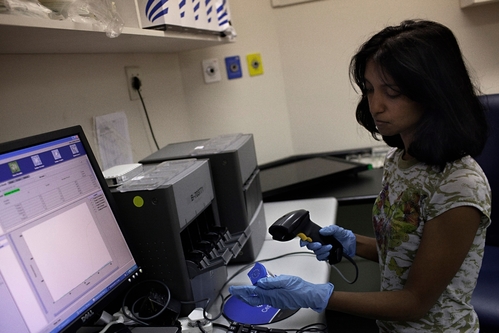
The diagnostic gap remains massive. Only seven countries[2] in the report have made Xpert MTB/RIF – a rapid molecular test to diagnose TB and test for resistance to first-line TB drugs – widely available. This means that the majority of people in the 29 countries surveyed are still tested with a method that fails to detect many cases or requires several months to confirm the disease.
This challenge explains why so many people remain undiagnosed and untreated; globally in 2015, based on the gap between estimated TB incidence and the actual number of cases reported, 4.3 million people with TB were never diagnosed.

“How are people supposed to get treated for TB when they’re not even getting diagnosed?” asked Dr Isaac Chikwanha, HIV and TB medical advisor at MSF’s Access Campaign. “If countries don’t do more to make sure that people can be tested, it will be impossible to reduce preventable deaths from TB.”
There has been progress in making available newer, more effective treatments that ease the burden for people with TB.
Staying in hospital for an extended period of time can limit a person’s ability to have a normal life and should be reserved for the sickest DR-TB patients. The report found that 34 per cent of the countries surveyed still require long-term hospitalisation for treatment of DR-TB.
Newer medicines for the treatment of DR-TB have demonstrated better outcomes than today’s regimens, which only offer a 28 per cent cure rate for extremely drug-resistant (XDR) TB and a 52 per cent cure rate for multidrug-resistant (MDR) TB.
Seventy-nine percent of countries surveyed include the newer drug bedaquiline in their national guidelines, and 62 per cent include delamanid. Yet globally, only five per cent of people who could have benefitted had access to these drugs in 2016.
DR-TB treatment, which in some cases requires swallowing nearly 15,000 pills over a period of up to two years, can now be shortened to nine months. Shorter treatments help people to resume a normal and productive life faster. But only 13 (45 per cent) of the countries[3] surveyed have made shorter treatments available.
“With TB, the clock is ticking rapidly, as every 18 seconds a person dies of TB. We have to change that,” said Sharonann Lynch, HIV and TB policy advisor at MSF’s Access Campaign.
“The number of people diagnosed over the last four years has stalled, while the number of deaths has increased rather than decreased. Countries need to use new tools and step up the pace of their response.”
The G20 governments are major contributors to the global TB response, with more than US$1.6 billion contributed to the Global Fund to Fight AIDS, Tuberculosis and Malaria in 2016. The G20 leaders now need to mobilise their resources to get more people diagnosed, make effective treatments accessible to all people affected by TB, and reduce TB deaths.
[1] Armenia, Afghanistan, Bangladesh, Belarus, Brazil, Cambodia, Central African Republic (CAR), China, Democratic Republic of Congo (DRC), Ethiopia, Georgia, India, Indonesia, Kazakhstan, Kenya, Kyrgyzstan, Mozambique, Myanmar, Nigeria, Pakistan, Papua New Guinea (PNG), Philippines, Russian Federation, South Africa, Swaziland, Tajikistan, Viet Nam, Ukraine and Zimbabwe.
[2] Armenia, Belarus, Brazil, Georgia, South Africa, Swaziland, and Zimbabwe.
[3] Afghanistan, Bangladesh, Cambodia, CAR, DRC, Kyrgyzstan, Myanmar, PNG, Philippines, Swaziland, Tajikistan, Viet Nam and Zimbabwe.
MSF has been treating people with TB for 30 years. In 2016, MSF treated more than 20,000 people with TB, including 2,700 people with multi-drug-resistant TB (MDR-TB).
The Stop TB Partnership and its 1,600 partners are a collective force that is transforming the fight against TB in more than 110 countries.



