Summary
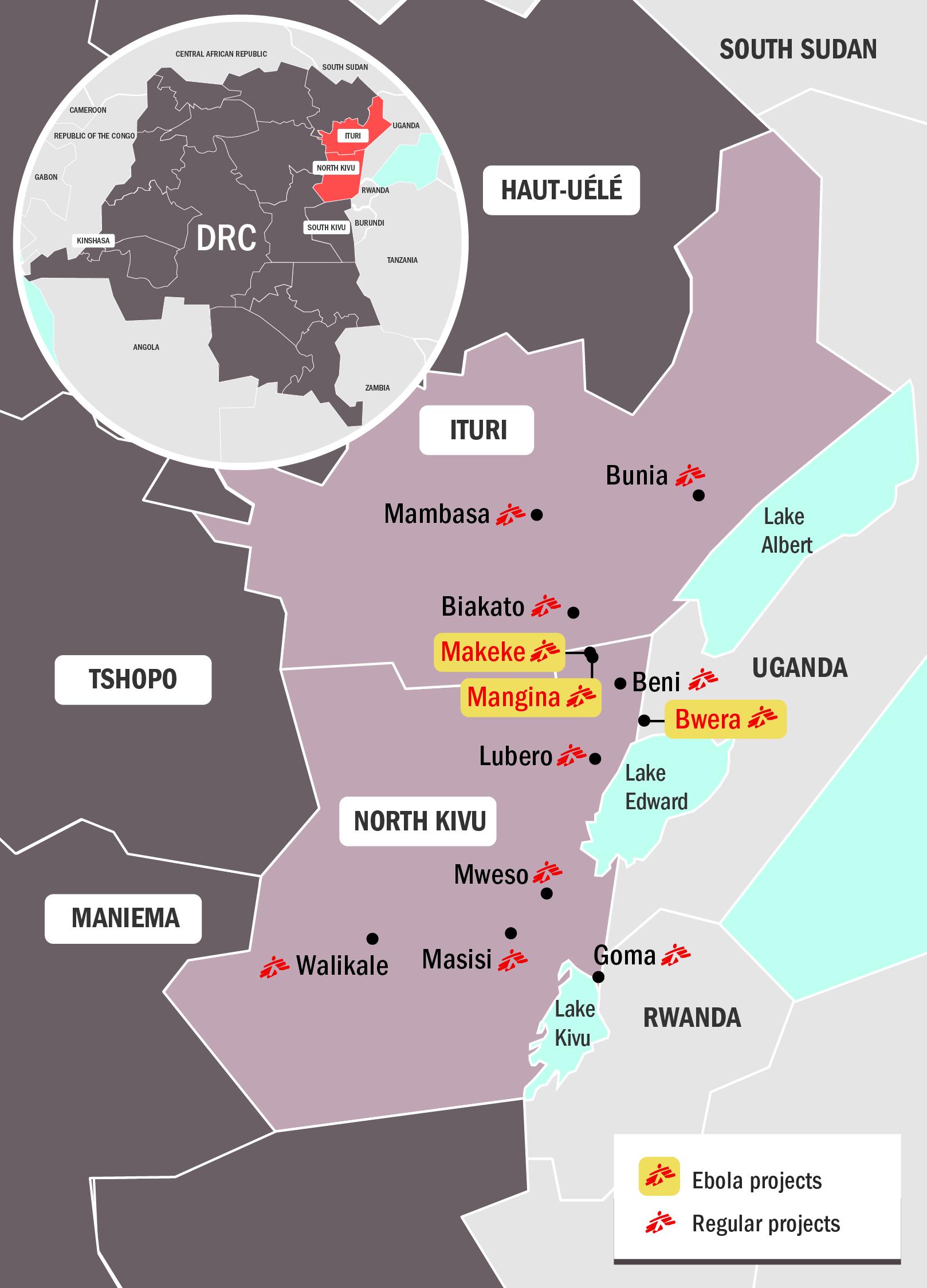
Democratic Republic of Congo (DRC) declared their tenth outbreak of Ebola in 40 years on 1 August 2018. The outbreak is centred in the town of Mangina, in the northeastern North Kivu province.
Latest figures - information as of 3 September 2018; figures provided by DRC Ministry of Health
91
91
14
14
51
51
Retrospective investigations point to a possible start of the outbreak back in May – around the same time as the Equateur outbreak earlier in the year. Although no connection between the two outbreaks can be established, it cannot ruled out either.
The delay in the alert and subsequent response can be attributed to several factors, including a breakdown of the surveillance system due to the security context (there are limitations on movement, and access is difficult) and a strike by the health workers of the area which began in May, due to non-payment of salaries.
The initial alert came after a woman from Mangina was admitted to the local health centre on 19 July for a heart condition. She was discharged but died at home on 25 July, after presenting symptoms of haemorrhagic fever. Members of her family subsequently developed the same symptoms and also died soon afterwards. A joint Ministry of Health/World Health Organization (WHO) investigation on site found six more suspect cases, of which four tested positive. This result led to the declaration of the outbreak.
The national laboratory (INRB) confirmed on 7 August that the current outbreak is of the Zaire Ebola virus, the most deadly strain and the same one that affected West Africa during the 2014-2016 outbreak. Zaire Ebola was also the virus found in the outbreak in Equateur province, in western DRC earlier in 2018, although a different strain than is affecting the current outbreak.
Current situation
Four weeks after the declaration of the epidemic, the epidemiological situation in Mangina and the surrounding areas is still concerning; four health zones in North Kivu and Ituri provinces - Mandima, Mabalako, Beni and Oicha - have so far reported confirmed or probable cases of Ebola. Teams are still working on identifying all active chains of transmission. This is not simple given that some cases have occurred in highly insecure areas and cannot easily be followed up with the usual case investigation and contract tracing.
Since the beginning of the outbreak over 4,100 contacts have been identified and more than 2,300 are being followed up by the Congolese Ministry of Health. The contact tracing and follow-up is done by the MoH with a team of epidemiologists.
Whilst cases have decreased dramatically, we cannot yet say that the epidemic has stabilised or is under control. New cases are still arriving at our treatment centre in Mangina but we are not seeing the number of suspect cases we would expect to see at this stage of the epidemic. We are concerned that this could be because patients experiencing symptoms are too afraid to access care or do not understand the importance of early hospitalisation and treatment. We also don’t have a clear idea about how many unreported deaths have occurred at community level.
| Confirmed cases | Probable cases* | Confirmed deaths | Health staff infected |
|---|---|---|---|
| 91 | 30 | 51 | 17 |
*Probable refers to community deaths that have links to confirmed Ebola cases but which were not tested before burial.
Area
Mangina, a town of 40,000 people, is in Beni Territory, North Kivu province, northeastern DR Congo. Beni, the administrative centre of the territory, is about 30 kilometres away and is home to about 420,000 people. The area borders Uganda to the east; the North Kivu capital Goma, and the Rwandan border are further south. This area sees a lot of trade, but also traffic, including “illegal” crossings. Some communities live on both sides of the border meaning that it is quite common for people to cross the border to visit relatives or trade goods at the market on the other side. The region is densely populated, and the Ugandan border is a sensitive area and is crucial in terms of developments of the outbreak spreading in the region.
The territory is characterised by high levels of insecurity – it is considered an area of conflict, with over 100 armed groups estimated to be active in North Kivu. Kidnappings and carjacking are very common. It is an area of heavy ongoing military operations – the city of Beni is subject to military rule and military justice, and moving around some areas in the region is quite difficult and sometimes impossible.
Existing MSF presence in the area
MSF has had projects in North Kivu since 2006. Today, we have regular projects along the Goma-Beni axe as follows:
- Lubero hospital: paediatric/nutrition care and treatment of sexual and gender-based violence.
- Bambu-Kiribizi: Two teams support local emergency room and paediatric and malnutrition in-patient departments, plus care and treatment of sexual and gender-based violence.
- Rutshuru hospital: MSF withdrew from the hospital at the end of 2017. However, in light of the volatile conditions in the region, we have returned to support emergency room, emergency surgery and paediatric nutrition programmes.
- Goma: HIV programme supporting four medical centres (including access to antiretroviral treatment).
The response to the current outbreak
The DRC Ministry of Health (MoH) is leading the outbreak response, with support from WHO. The MoH team sent to coordinate the response in Beni was dispatched from Kinshasa and is the same team that coordinated the response in Equateur province. The WHO emergency pool was mobilised in the area upon the declaration of the outbreak.
Epidemiological surveillance is being set up both in North Kivu and Ituri provinces and a laboratory for testing is fully operational in Beni (previously every sample was sent to Kinshasa). Other partners are involved in water and sanitation, health promotion and community outreach activities.
On 7 August the Ministry of Health announced they will start vaccination of their health workers on the following day.
MSF response
At the MoH’s request, MSF is part of the task force coordinating the intervention. Our teams are focusing on caring for patients affected by the virus, as well as protecting local health structures (and their workers) by helping with triage, decontamination and training.
In total, 337 staff are currently working in MSF’s Ebola projects in North Kivu and Ituri provinces.
MSF's first task was to improve an isolation unit for suspect and confirmed cases in the Mangina health centre, the epicentre of the outbreak, where patients were isolated and cared for whilst a treatment centre was built. A treatment centre was subsequently opened on 14 August, with a capacity of 68 beds which can bed extended to 74 beds if required.
Teams have been progressively increasing the level of supportive care (oral and intravenous hydration, treatment for malaria and other co-infections, as well as treatment of the symptoms of Ebola), and have also been able to offer new therapeutic treatments to patients with confirmed Ebola infection under the MEURI protocol. These treatments are given only with the informed consent of the patient (or a family member if they are too young or too sick to consent) and are provided in addition to supportive care.
As of 3 September, MSF had treated 65 patients confirmed to have Ebola and admitted a total of 124 patients for testing for the virus in Mangina. Of the patients confirmed Ebola-positive in Mangina Ebola Treatment Centre, 29 had recovered and returned to their families; three confirmed patients and two suspect patients remained under treatment.
Another isolation centre was built by MSF in Beni and handed over to the Ministry of Health, who assigned it to another NGO; it is now a treatment centre.
MSF teams also built a 7-bed transit centre in Makeke (on the North Kivu-Ituri border), which was opened on 28 August. The centre allows suspect patients to be isolated and tested for the virus. If they test positive, they are transferred by road to one of the treatment centres in either Mangina or Beni. It is hoped the transit centre will help overcome resistance to the Ebola response in the community.
Health centres in Mangina and Beni that have seen positive cases are also being decontaminated. MSF teams are working in the Beni and Mangina areas, as well as in Ituri between Mambasa and Makeke (on the border with North Kivu), visiting health centres and training staff on the proper triage of suspected Ebola patients. Our teams are also training staff on setting up isolation areas in case of need.
MSF has recently received authorisation to begin vaccinating frontline workers (health staff, religious leaders, burial workers, etc) from Makeke on the North Kivu-Ituri border up to Biakato. Given that the population from Mangina often move in this direction, it is hoped that vaccination will help to stop the infection spreading further into Ituri province.
Our teams in Uganda have also been mobilised to be ready in case the outbreak spills over from across the border. They have installed an isolation tent in Bwera, a small town directly over the border from Beni and Butembo. MSF's non-emergency project in Hoima (Uganda) has also set up an isolation tent.
All MSF projects in North Kivu and Ituri areas have been supplied with Ebola equipment, including personal protective equipment (PPE), and have put proper hygiene and infection control protocols in place to safeguard staff and patients from the risk of contamination, should the epidemic spread further.







