More than six months into the beginning of the latest Rohingya exodus, people continue to flee from Myanmar into Bangladesh fearing for their lives and seeking safety. A total of 3,236 refugees are reported to have entered Bangladesh in February alone, bringing the total number of new arrivals in 2018 to more than 5,000, according to UNHCR. They add to the nearly 700,000 that have reached Bangladesh since 25 August, and to the more than 900,000 total refugees, including those arrived over different periods of tension in Myanmar.
Summary
Number of health facilities
10 health posts; 4 primary health centres (open around the clock); and five inpatient health facilities (providing 24-hour secondary healthcare).
Number of staff
To respond to the fastest-growing refugee crisis in the world, MSF’s team in Cox’s Bazar has increased 10-fold in the past six months to more than 2,800 staff – the majority of them Bangladeshi nationals.
Number of patients
Over the past 6 months, our teams carried out 351,421 outpatient and 8,135 inpatient consultations.
Main morbidities
Respiratory infections, diarrhoeal diseases, skin diseases – all related to poor living conditions.
Water and sanitation
This is key to prevent the spread of disease. Activities include drilling boreholes and tube wells, installing a gravity-fed water supply system, trucking in water, desludging old latrines, constructing new sustainable latrines, doing bucket chlorination and distributing domestic water filters.
Mental health services
This has been scaled up, with more counsellors added to existing teams, services available at additional health posts, and training outreach workers to provide basic psychosocial support.
Outreach
Teams focus on health promotion, outbreak prevention, alert and response, while a surveillance team gathers demographic, nutritional, mortality and natality indicators, covering 80% of the refugees’ settlements. The teams also do active case-finding and referral to health facilities for diagnosis and treatment, as well as defaulter tracing and mobilisation for vaccination. An all-female team spreads messages about sexual and reproductive health in the community.
Current health concerns
Seasonal threats
The area where refugees are living is prone to cyclones and heavy rain that could potentially destroy temporary shelters and displace a large number of people. Natural disasters such as floods, tropical cyclones, hurricanes, storm surges and tidal bores are frequent in the coastal belt of Bangladesh, which includes the Cox’s Bazar district.
The upcoming rainy season brings with it the risk of respiratory tract infections, effects on mental health and the exacerbation of existing illnesses, as well as waterborne diseases such as acute watery diarrhoea, typhoid, hepatitis, shigellosis or mosquito-borne diseases such as malaria and dengue fever.
Acute jaundice syndrome
Since December, MSF has seen 1,259 patients with acute jaundice symptoms, which commonly cause a yellowing of the skin and eyes, and may indicate that a person has hepatitis. Suspected cases are tested, while water and sanitation teams assess facilities in the area and respond as needed.
Non-communicable diseases
MSF currently offers clinical stabilisation and management of acute, life-threatening exacerbation of diseases such as asthma, diabetic, hypertension, and chronic obstructive pulmonary diseases. However, MSF is struggling to address continuation of care for patients with non-communicable diseases, which require proper referral pathways, facilities, laboratory follow-up and human resources, all of which still need to be put in place.
Sexual and reproductive health
MSF is intensifying its activities focusing on mother-and-child and reproductive healthcare. Only a minority of expected deliveries occur in a health facility, while home deliveries often happen in unsafe and unhygienic conditions. Moreover, MSF sees many women and girls seeking medical care for pregnancies which are the result of rape. The lack of support mechanism for rape-related pregnancy can have dangerous consequences, such as unsafe abortions and death. Some rape-related pregnancies are quite advanced and women are unable to return to their community. MSF refers these women and girls to a safe shelter under the care of a dedicated organisation, although existing capacity in the camp is extremely limited.
Mental and psychosocial health
The mental and psychosocial impact of being forcibly displaced and living in such difficult conditions continue to affect the Rohingya refugees. Mental health services remain an important part of MSF assistance to people who have experienced extremely high levels of violence, as confirmed by the retrospective mortality surveys we published in December.
Measles
Between September and the end of February, we saw 4,370 cases of measles across all the MSF health facilities. Cases are now decreasing although the outbreak is far from over. Vaccinating all children under five years newly arriving in the camps against measles remains one of MSF’s top priorities. Two rounds of a mass vaccination campaign were organised by the Minitry of Health with MSF support.
Diphtheria
MSF has treated more than 4,678 people for diphtheria in the Cox’s Bazar district as at the end of February, with most of patients aged between five and 14 years. During the peak of the outbreak, MSF ran three dedicated health facilities. At Rubber Garden, MSF has set up a dedicated diphtheria treatment centre and follows up throughout the settlements with the family members and other people who have been in contact with the patients. These contacts are treated preventatively with antibiotics via an outreach team who follow up to ensure the medication is taken on a daily basis. The contacts are also sent to the health post to get vaccinated against diphtheria. An MSF team is also responsible to trace patients after 30 days from the date of admission to ensure medical care for post-diphtheria complications is received. Any person who reports having symptoms indicative of post-diphtheria complications or other illness are referred to MSF’s health facilities for a clinical assessment. Then appropriate treatment is given or patients are referred to other health care providers who offer palliative or rehabilitative services if needed. The Government of Bangladesh is implementing a vaccination campaign against diphtheria.

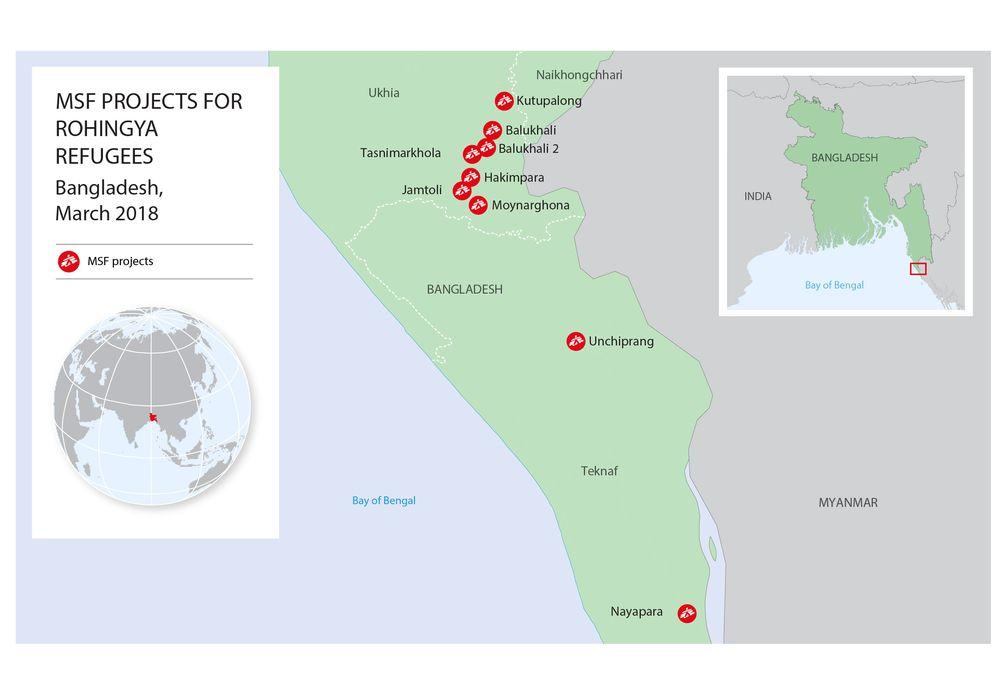
MSF project locations in Cox’s Bazar
Rubber Garden
Close to Rubber Garden transit centre for new arrivals, near Kutupalong Makeshift Settlement, MSF opened a dedicated diphtheria treatment centre in response to an outbreak of the disease. The treatment centre opened on 27 December and now has 35 beds for patients with diphtheria and capacity to increase up to 70 beds if needed. In order to reduce the spread of the disease, the team is also involved in active case finding, contact tracing (finding the patient’s household, ensuring the prophylactic treatment is completed) and follow-up. Patients are traced by the MSF outreach team after 30 days from the date of admission have passed to ensure medical care for post-diphtheria complications is received. Moreover, as part of our preparedness plans for potential outbreaks, MSF is increasing the capacity of the facility and improving awareness of the signs and symptoms of a number of diseases among the local population and refugees in coordination with other organisations.
Kutupalong - Balukali
Nearly 600,000 refugees are living in Kutupalong and Balukhali area, also known as the Megacamp.
Kutapalong
This facility has been operating since 2009 and is the largest MSF health facility in Cox’s Bazar. Services in the clinic include a 24-hour emergency room, an outpatient department (OPD), an inpatient department (IPD), including paediatric and neonatal wards, isolation beds, a diarrhoea treatment ward, sexual and reproductive healthcare services including 24 hour care for survivors of sexual violence, a mental health department, and basic laboratory services including blood transfusion for life threatening emergencies.
Since 25 August, the IPD has been expanded from 50 to 79 beds to cope with the influx and the increasing numbers of patients. Isolation capacity was also expanded due to the potential outbreak of communicable diseases. In order to increase the number of beds available and improve the overall infrastructure in the hospital to meet the needs of the growing population, construction works are ongoing; a temporary OPD was opened on 24 December to be used as temporary site until a new and larger OPD is finished. The OPD currently treats over 300 patients per day. MSF is also currently expanding maternity, sexual based violence, new-born, and paediatric care activities. Renovation and future expansion of the inpatient buildings are ongoing to reach a patient capacity of 110 beds.
MSF runs three health posts throughout the settlement in Kutupalong Makeshift Settlement (KMS) Expansion area to provide basic primary healthcare. The health posts in total treat over 300 patients per day. They will be used as fixed vaccination sites for EPI (The Expanded Programme on Immunization).
Balukhali
An inpatient facility in Balukhali had been functioning as a diphtheria treatment centre with 75 beds since early December, leaving only the ER functional for other morbidities. On 12 January the facility changed back to a mother and child healthcare facility. Services include paediatrics (15 beds) and neonatal care/inpatient therapeutic feeding centre (ITFC) (15 beds), maternity (10 beds), emergency room and observation (5 beds) and an isolation ward (20 beds). MSF also runs two health posts and an outpatient facility in the settlement to provide basic primary healthcare.
Health posts will be used as fixed vaccination sites for EPI, following the completion of the third round of diphtheria vaccinations. During the month of February, teams carried out over 10,000 outpatient consultations.
Balukhali 2
MSF has been running two health posts in Balukhali 2 providing basic primary health care. Each health post treats over 200 patients per day. Services in this health post include an outpatient department (OPD) and sexual reproductive healthcare services (antenatal, postnatal, sexual-gender based violence, gynaecological consultations and family planning).
Tasnimarkhola
There are over 58,000 refugees living in Tasnimarkhola makeshift settlement, formerly known as Burma Para. MSF opened a health post on 26 October and has treated over 25,000 patients between the opening and the end of February. Around 25 percent of consultations are for children under five. In December, MSF started sexual and reproductive health activities (antenatal, postnatal, sexual-gender based violence, gynaecological consultations and family planning).
On 26 November, MSF opened an inpatient facility with an emergency room and a 50-bed capacity. During the diphtheria outbreak, measles cases (children) were referred there. Afterwards, the hospital extended services from paediatrics to include adults.
Moreover, MSF has completed the drilling of 10 deep production boreholes to provide water to the health posts and IPD.
In addition to the ongoing activities, at the beginning of April, MSF is planning to open a 100-bed inpatient facility located within the Balukhali makeshift settlement within the mega camp, Kutupalong. The semi-permanent structure will include a 24-hour emergency room, adult and paediatric ward, intensive care unit, isolation beds, a 50 bed isolation unit in case of outbreak, maternity with sexual and reproductive healthcare services, non-communicable disease (NCD) care and follow up, a comprehensive laboratory service and an ambulance referral system.
Unchiprang
There are over 22,000 refugees living in Unchiprang makeshift settlement. MSF has been running a primary health centre, which was initially opened as health post in mid-September. It is the main health-care provider in the settlement and the team is carrying out around 250 consultations per day. The structure includes a 24-hour emergency room and maternity ward with sexual and reproductive healthcare, mental health services, and an isolation facility. The teams also do active case finding and referral to health facilities for diagnosis and treatment, as well as defaulter tracing and mobilisation for vaccination.
Nayapara
There are over 23,000 refugees living in Nayapara refugee camp together with an estimation of around 13,000 households in the informal settlement around the camp. MSF has been running a primary health centre that includes an emergency room with referral capacity, an outpatient department (OPD), with sexual reproductive healthcare and mental health services. The team is carrying out around 250 consultations per day.
Jamtoli
There are around 55,000 refugees
living in Jamtoli makeshift settlement. MSF has been running a primary health centre that include a 24-hour emergency room, an outpatient department (OPD), a paediatric and an adults ward, sexual reproductive healthcare, sexual and gender-based violence (SGBV) and mental health services. The clinic is currently seeing around 280 patients per day and offers a 24-hour primary health care service, with a delivery room, 10 hospitalisation beds, 10 isolation beds and an ambulance referral system. MSF’s outreach teams focus on health promotion, outbreak prevention, alert and response, while a surveillance team gather demographic, nutritional, mortality and natality indicators.
Hakimpara
There are around 34,000 refugees living in Hakimpara makeshift settlement. MSF has been running a primary health centre that include a 24-hour emergency room, an outpatient department (OPD), a paediatric and an adults ward, sexual reproductive healthcare, SGBV and mental health services. The clinic is currently seeing around 150 patients per day and offers 24-hour primary health care service, with a delivery room, 13 hospitalisation beds, 10 isolation beds and an ambulance referral system. MSF’s outreach teams focus on health promotion, outbreak prevention, alert and response while a surveillance team gather demographic, nutritional, mortality and natality indicators.
Moynarghona
There are over 22,000 refugees living in Moynarghona makeshift settlement. MSF started a mobile clinic in September, which has since been upgraded to a health post. The team is carrying out nearly 160 consultations per day on average. Services in this health post include emergency, an outpatient department (OPD), including a paediatric ward, sexual reproductive healthcare and mental health services. In February, MSF opened an inpatient department (IPD) with 63-bed capacity including a paediatric and neonatal ward, isolation beds, a diarrhoea treatment ward, sexual and reproductive healthcare services, a mental health department, basic laboratory services and an ambulance referral system. This facility was under construction in December when the diphtheria outbreak led the organisation to temporarily transform it into a Diphtheria Treatment Centre until mid-February.
Sabrang entry point
At the border point in Sabrang, MSF started a mobile clinic on 8 October, offering nutritional screening and basic primary health care and monitoring, whose services have been integrated in the circuit of the reception centre. The daily mobile clinic situated in Sabrang entry point screens and provides consultations to all new arrivals. Mobile clinic services include OPD consultations – adult and paediatric, identification of severe cases, psychological first aid and referrals.

Other activities
Vaccination
The coverage for routine immunisation is low. This, combined with crowded living conditions, a lack of adequate water and sanitation, and little access the Rohingya population had to routine healthcare in Myanmar represents a public health risk to both the new arrivals and the host population. MSF is supporting the government in expanding routine vaccination in the camps through initiating vaccination for children and pregnant women at MSF facilities. Staff at all MSF health facilities will have the capacity to administer immunisation for measles and rubella, oral polio, pneumococcal conjugate vaccine (PCV), pentavalent vaccine and tetanus according to national protocols. With the support of other actors, the Ministry of Health and Family Welfare has been implementing a measles and diphtheria vaccination campaign. MSF has been supporting this by setting up fixed points in our health posts or supporting with human resources.
Sexual violence
From the end of August 2017 to the end of February 2018, MSF has treated 226 survivors of sexual violence at MSF’s Sexual and Reproductive Health Units. Most of them (162) were rape survivors. Over half of the survivors are under the age of 18, including three nine-year-old girls. Given these barriers, it is likely that the number of SGBV survivors MSF has treated so far is just a fraction of the real figure. MSF has specialised staff on the ground to treat survivors who are referred for treatment as a result of trauma, including sexual assault and rape. MSF’s local community outreach workers visit people living in the settlements, informing them about the free services the organisation offers, including treatment for sexual violence. At our clinic, we offer these women comprehensive health care, including mental health counselling. We also discuss possibilities and support options with them, based on their individual needs.
Water and sanitation (WASH)
Outside of the medical response, improving water and sanitation is a major part of our work to prevent the spread of disease. Emergency facilities that were put up quickly in the first phase of response have been of low quality, requiring decommissioning or rehabilitation, as do thousands of poorly placed and low-quality water systems. With the on-going influx, congestion is a major concern; overburdening existing facilities and complicating access for emptying latrines thus increasing the public health risk in these sites. Desludging and decommissioning of these latrines remains a priority to improve the inadequate sanitation environment. MSF is supporting the activities with a major focus on water and sanitation: 254 latrines were dismantled so far. Considering that the shallow aquifer is contaminated with fecal coliforms throughout the camps, MSF has been drilling since November deep production boreholes up to 150-200 metres deep to have clean water to serve piped networks to reach between 5,000 to 30,000 people.

So far MSF has built 1,522 latrines - serving around 30,000 people every day with an appropriate toilet – and provided clean water to between 65,000 and 130,000 people. Both in the settlements located in the north as well as in the ones in the south, 262 water wells have been built and a distribution system has been implemented to deliver water with the appropriate quality, quantity and pressure flow.
The availability of safe drinking-water is an increasing major concern in the settlements and outbreaks of water-borne diseases are inevitable (acute, watery diarrhoea, hepatitis E, typhoid), given the scale of the population together with the worsening environmental conditions. To ensure access to clean drinking water, MSF is doing assessments of water sources, soap distribution (roughly 1,153 households), hygiene promotion messaging and bucket chlorination at water source (35 bucket chlorination points). MSF is also distributing domestic water filters both in our clinics in Tasnimarkhola and Balukali 2 to patients suffering from malnutrition, measles and diarrhoea and in general to children under five and pregnant women, and in specific areas where water-borne diseases are identified.
MSF also includes water supply and sanitation in its emergency response for new arrivals. MSF has deployed teams to arrival, transit and settlement locations to ensure that newly-arrived refugees have access to safe drinking water and adequate sanitation facilities.






