Since 2012, 60,000 Haitians from all walks of life have benefited from free, first-class surgical trauma care through MSF’s Nap Kenbé hospital in the Tabarre neighbourhood of Port-au-Prince.
Opened in response to the earthquake in 2010 and the resultant spike in acute medical needs, MSF is gradually reducing its activities in the hospital and preparing for closure by mid-2019 so as to reallocate its resources according to current needs, in Haiti or elsewhere.
We take a look at what has been achieved in one of MSF’s most advanced surgical projects and hear from some of the patients who have benefited.
12 January 2010: the earth shatters in Haiti. Within a few seconds, the capital city is flattened. Over 100,000 die and thousands upon thousands are injured or trapped in the rubble.
“In terms of consequences for the local health system, it’s similar to a large epidemic; but one caused by injuries instead of an infectious disease,” explains Dr Miguel Trelles, MSF surgical advisor. This spike in acute medical needs happened right at a time when the country was the least able to treat the wounded, as its medical infrastructure had been destroyed or was in disarray after the catastrophe.
Faced with the scale and long-lasting impact of the disaster, MSF decided to open one of its first and most advanced trauma hospitals in Port-au-Prince. The organisation was already managing a trauma aisle in Port-au-Prince’s Trinité hospital, but it was flattened by the quake. It was also too small to meet the demand for such services, which soared even after the ‘epidemic of injuries’ had subsided, as a result of violent trauma and road accidents among other things.
A surgical success story
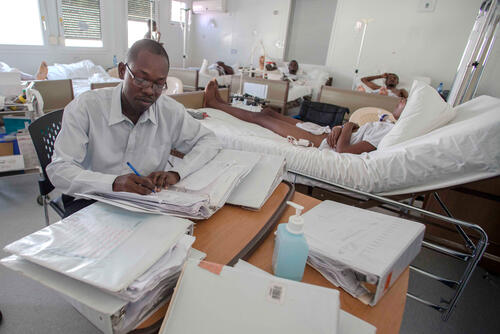
Nap Kenbé hospital, a temporary structure built on containers in the Tabarre neighbourhood of Port-au-Prince, opened its 107 beds on Valentine’s Day in 2012 and offered, for free, first-class surgeries that were before only available to the richest Haitians through the private sector.
The hospital was quickly a victim of its success: within less than a year, the number of surgical interventions was twice the original plans, and demand kept growing, mainly from victims of accidental injuries such as traffic accidents.
In its six years of existence, Nap Kenbé hospital has treated 60,000 Haitians from all walks of life, providing emergency trauma and visceral surgeries with often long physiotherapy follow-up required to ensure full recovery and use of limbs.

Eight years after the earthquake, the emergency phase is clearly over and MSF, as an emergency organisation, is preparing to close its hospital by mid-2019.
By that time there should be additional capacity to take over trauma care in Port-au-Prince, including the scheduled reopening of the Hopital de l’Université d’Etat d’Haïti (HUEH). With over 500 beds, the HUEH was the largest hospital in the country. It was destroyed during the quake but, with strong support from other international partners, its rehabilitation is nearing completion.
First-class fracture treatment
Internal fixation is one of the services provided, for free, at Nap Kenbé hospital.
In high-income countries, it is a routine procedure for closed fractures (i.e. where the skin has not been broken); it was routinely used to treat the wounded after the large 2011 earthquake in Japan, for example.
Besides making recovery less painful, internal fixation speeds the recovery time and shortens the hospital stay. But it is a costly procedure and was not available in Haiti.
The alternatives (for example using plaster or traction) require the patient to be immobilised, in hospital, for six weeks. This was a challenge following the Haiti earthquake, the most devastating in living memory: not only there were more people in need of hospitalisation than there were beds available in Port-au-Prince, but each patient needed to stay a very long time in those too few hospital beds.
Internal fixation not only requires specific equipment and trained staff; it also carries too high a risk if not performed in perfect infectious control conditions – the risk of bone infection. “If surgery and hospitalisation conditions are not optimum, using internal fixation can do more harm than good,” Dr Trelles explains.
Most low-resource countries where MSF traditionally works and has often provided emergency trauma care following natural disasters (Haiti, Indonesia and Nepal, to name but a few) have weak health systems and underfunded health facilities. It is not recommended to perform internal fixation in such situations, so MSF mostly uses traction or casts to treat patients with closed wounds.
For MSF, Nap Kenbé hospital was a training ground to improve its intensive care unit management and improve its protocols for internal fixation. And from 2014 onwards the organisation trained 24 Haitian orthopaedic doctors and future surgeons each year as part of a residency programme.
“I can rely on my hand again”
Nine-year-old Derlens lives with his mother, who runs a small stall in in Port-au-Prince’s main market. His life was turned upside down on 25 July 2017, when he almost lost his right hand and forearm doing a few odd jobs for some bakers who had set themselves up in a yard next to his house.
“I was only distracted for a moment, but my arm was already crushed,” says Derlens. “I shouted out so everyone would realise my arm was stuck in the machine.” He was taken to the Martissant emergency centre (managed by MSF) and was transferred from there to Nap Kenbé hospital in Tabarre.
“After the accident I was very scared. I thought I was going to lose my hand. But when I arrived at the hospital, a nurse gave me hope. Now I’m healed and I find I can rely on my hand again,” says Derlens. After two months of hospitalisation and three months of rehabilitation, he has regained most of the function in his hand, despite being left with a noticeable scar.
“A surgical operation like this one would have been impossible for us to afford in a private clinic. Look! I’m here with Derlen because his mother can’t even come with him to medical check-ups because she has to go and find food for her kids,” explains Guerdline, Derlens’ cousin, who has accompanied him to his physiotherapy session.

A bullet in the leg in the name of revenge
“I didn’t get this bullet in my leg during a fight or a scuffle. It was my best friend’s boyfriend. He was part of a notorious group of bandits operating in our community,” says Cheldine, 17, coolly. “I had tried to explain to my school friend that she didn’t realise who he really was. Unfortunately, she told him what I’d said, and he vowed to take revenge on me.
“I bumped into him at a big crossroads, one afternoon when I was leaving school. He took out his gun in front of everyone and shot a bullet into my left leg. I gathered all my strength and didn’t cry, despite the blood running to the ground and the people panicking around me.
“Frustrated and aware they couldn’t question him, the people who lived nearby came with me to the MSF clinic in Martissant, which is not too far from my neighbourhood. In the meantime, others told my mother to meet me there in the emergency centre. It was the first time I’d set foot in an MSF hospital. I already knew that services were offered for free. But I didn’t know all the care was free: I didn’t have to pay for medicines, radiography or lab exams.”
“It was already difficult for me to pay for transport so I could visit Cheldine in hospital. I don’t know what I would have done if I’d had to pay [hospital] bills,” Mrs Jean Pierre, Cheldine’s mother, adds.

“I was hit by the projectile when I was in bed.”
Sophonie, 32, was hit by a stray bullet while she was lying in bed. “It was a little after 9pm,” she explains. “I wasn’t yet asleep when I felt something hit me right in the stomach. It was hot, and it hurt a lot. I rubbed the spot and realised that it was bloody. My boyfriend tried to give me some first aid, then I ran into the street to grab a motorbike to get to hospital.”
“Once I’d reached the hospital, a private one, the staff gave me an intravenous infusion and advised me to go to MSF’s hospital in Tabarre because, according to them, my injury required specialised surgery that they weren’t able to offer. My partner had arrived in the meantime, and then an ambulance took me to MSF’s Nap Kenbé hospital. Of course I had a little money but I couldn’t pay for care at that level. And I didn’t want money to make the difference between life and death.”
“I explained what had happened, and then I fell unconscious. It was if I had just been hit by the bullet. When I woke the next day, a nurse explained that I had been operated on, but that the doctors had decided not to touch the bullet because of how close it was to my heart. I followed the necessary treatment until I left the hospital after two weeks. Now I return regularly to the outpatient clinic for radiography. They tell me that the bullet hasn’t moved a millimetre. But it’s still possible that it might, which causes me great stress. I also have respiratory problems that are getting more and more serious. I’m haunted by the idea that someone will tell me one day that my days are numbered. I have to talk about this often with my only daughter so that she won’t suffer a terrible shock if I must leave her one day.”
Sophonie sighs as she explains: “Since all this I’ve fallen into deep despair. I was no longer able to sleep in my room. I had to escape from it, and went to live in another neighbourhood. I knew that anything could happen in this country, but I still can’t believe that something like this could happen so easily. I’m not living in anger about my situation, but I remain frustrated, continually asking myself, ‘Why did this happen to me?’”







