1. One of the world’s least developed countries
Political instability in Guinea-Bissau has had a significant impact on the health system.
A lack of resources and qualified personnel, and the practical nonexistence of a referral system, limits the population’s access to good quality basic healthcare services.
The situation is exacerbated further by the lack of prevention activities and effective epidemiological vigilance.
Children under the age of five and pregnant women are the first affected. Despite the presence of international humanitarian organisations and the implementation of various medical programmes, a large number of people do not have access to healthcare.
In this context, MSF has opened a paediatric care project in the country’s main hospital, Simão Mendes National Hospital (HNSM), where it manages the paediatric emergency unit, as well as the paediatric and neonatal intensive care units, and an inpatient therapeutic feeding unit.

2. The most serious cases first
Respiratory infections, malaria, diarrhoea and meningitis are the main diseases affecting children under five in Guinea-Bissau.
All are potentially fatal but, generally speaking, the prognosis is good if adequate care is received quickly. However, like many health centres in the country, without MSF’s support the HNSM did not have the resources or qualified medical staff to respond to and manage critical cases effectively.
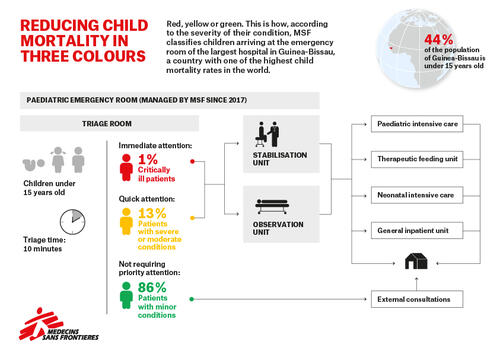
Our starting point was to establish a good triage system in the paediatric emergency unit. By classifying patients that come to the HNSM as green, yellow or red cases, children under the age of 15 are quickly referred to the appropriate services.
Now, the medical staff can guarantee faster and more efficient treatment, improving the care given to their youngest patients and reducing mortality.
3. From the most basic care to more sophisticated treatments
Despite being a reference medical centre, the HNSM does not fulfil its role as a tertiary referral hospital, i.e. a hospital offering the most advanced, specialised treatments.
Our priority at the start of the project was to put in place good basic medical care. Following rigorous protocols and correct treatment procedures are minimum standards that were previously not met and have a great impact on infant mortality in cases as serious as those treated in intensive care units.
From this quality basic medical care, MSF has been able to move towards more technical or sophisticated treatments, which require better trained medical staff and more specialised equipment.

4. Better trained medical staff
Medical care in units specifically dedicated to serious and critical paediatric cases is particularly complex and demanding. It requires specific medical skills and a higher ratio of medical staff to patients than in non-intensive hospital departments.
In a country like Guinea-Bissau, where there is no option for paediatric specialisation at university, this poses an even greater challenge: all the doctors we work with at the national hospital are general practitioners.
Training is one of the main pillars of the response, and a decisive element of our project at the HNSM. We send expatriate paediatricians to offer training to local doctors, and have nursing and medical university students attend the hospital to do shifts in the emergency room and intensive care units.

5. Close collaboration with the Ministry of Health
MSF’s presence in the paediatric services of the HNSM helps the Ministry of Health in its management of the department.
It has also revealed a series of problems in other departments. For instance, some serious paediatric cases could have been avoided if adequate reproductive healthcare had been offered. Many of the medical complications faced by newborns up to 28 days old originate from the delivery.
Therefore, given that many of the newborns treated in the paediatric emergency unit come from the hospital’s maternity ward, close contact must be maintained between the two departments.
In addition, a high number of children admitted to the intensive care unit at the HNSM have complications related to advanced-stage HIV infections. MSF therefore works with the Ministry of Health to mobilise resources, both human and financial, and enhance prevention efforts in this area.





