Introduction
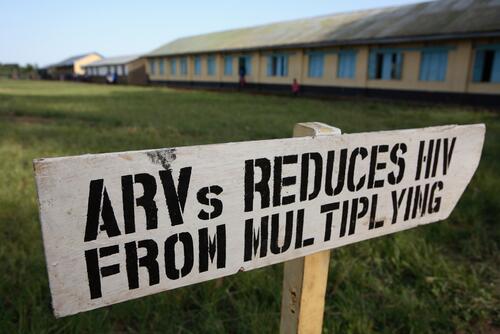
Médecins Sans Frontières (MSF) began providing antiretroviral treatment (ART) for HIV/AIDS in 2000 in Thailand, Cameroon, and South Africa, to a limited number of people in urgent need of treatment. At the time, doctors and nurses faced very sick patients in over-crowded waiting rooms. Initially providing treatment in dedicated HIV/AIDS projects, MSF has increasingly decentralised HIV services, including prevention, treatment and care, into primary health care facilities and partnered with health ministries to deliver care.
Over the past decade, we have witnessed time and again how treatment dramatically reduces illness and deaths in the communities in which we work. Today, MSF treats more than 170,000 people in 19 countries, and some MSF projects have been able to reach and maintain so-called ‘universal access’ to treatment in their districts.
Looking beyond MSF, the past ten years have seen considerable progress. The major mobilisation of donors triggered by UN Secretary-General Kofi Annan’s call for a “war chest” to fight the epidemic ushered in an unprecedented international effort to provide care and treatment in some of the most impoverished and hardest-hit countries in the world. The Global Fund to Fight AIDS, Tuberculosis and Malaria was created in 2002, followed by the US Government-led President’s Emergency Plan for AIDS Relief in 2003. Together, they provide treatment to 81% of the more than six million people who are alive today because of antiretroviral therapy (ART).
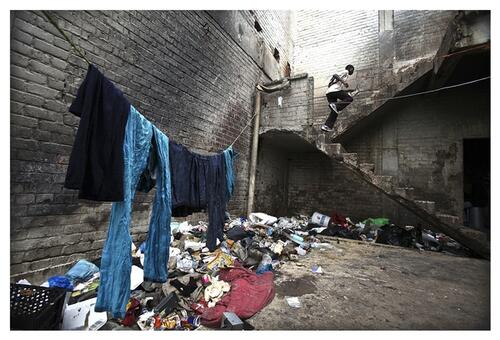
This is important progress – but the treatment gap endures. An additional ten million people are today still in urgent need of treatment and many will die within just a few years if left untreated. Recognising this, UN Secretary-General Ban Ki-Moon recently called for at least 13 million people to be on treatment by 2015. Others have asked for treatment targets to be set at 15 million.
MSF and other providers of care have learned important lessons about how to reach more people with treatment without compromising quality of care. By scaling up ART to more people in need, illness, deaths, and new HIV infections can be reduced. And by scaling up intelligently, and with the right policies, the costs associated with HIV care can be reduced, allowing more people to be reached. Today, the latest evidence is beginning to show that ART not only saves lives, but also can prevent transmission of the virus from one person to another. HIV treatment is therefore also HIV prevention, and can help slow the pace of the epidemic.
This report will detail MSF’s experience implementing treatment strategies to improve care and reduce costs for patients and health systems. It presents results of a survey conducted by MSF teams in 16 countries where MSF works.II The 16 countries represent a mix of low, general and hyper-endemic countries, and together account for 52.5% of the global HIV/AIDS burden.
The progress they have achieved in implementing WHO treatment guidelines as well as other important strategies to increase access to treatment, provides an important window into the current strengths and weaknesses of the international response to HIV/ AIDS. Most countries have policies to better manage the co-epidemics of HIV and TB; to integrate HIV and maternal services; and to bring care closer to where people live, using existing facilities and health care workers. But most HIV-prevalent countries are still struggling to reach more than 50% of people in need of ART or provide ART in more than 50% of existing facilities.
The progress thus far would not have been possible without external financial support, but it will take more mobilisation of domestic and external resources so that the population benefits of ART in reducing infections, deaths, and illness can be fully realised. With more than six million lives saved there is a lot to show for the last ten years of effort. But with new evidence of ART as prevention, even more can be done in the next decade.
As governments meet to draw up the blueprint for the next decade of the global HIV/AIDS response at a UN High-Level Meeting in New York in June 2011, they must recommit to their past promises to bring life-saving treatment to all in need, support an ambitious treatment target, and ensure the policies are in place to improve the quality of care, reduce the burden on patients and on health systems, support lowering the costs of drugs, and foster the needed medical innovation.