60,600
60,6
21,400
21,4
13,200
13,2

8,900
8,9
3,700
3,7
1,000
1,
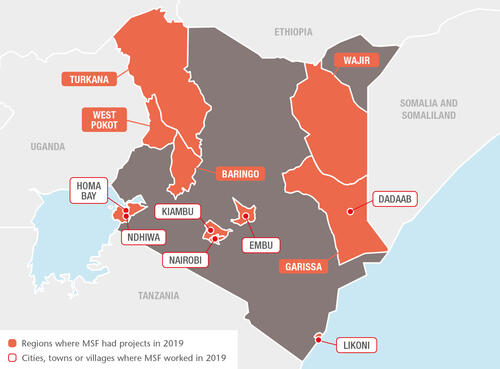
Kenya is MSF’s largest programme outside a conflict zone or emergency crisis. In the sprawling slums of Nairobi and in the three-decade-old Dadaab refugee camp, for example, many people still struggle to obtain effective diagnosis and care for life-threatening diseases.
Treating non-communicable diseases
Since 2017, we have been working in Embu to integrate management of non-communicable diseases into general healthcare facilities. In that time, more than 4,000 patients with non-communicable diseases have enrolled for treatment. In August, the second cohort of 18 trainees taking part in our staff mentoring scheme graduated, having successfully completed their modules. They are now able to manage patients with non-communicable diseases independently.
We support the adult medical wards (90 beds) in Homa Bay county referral hospital. In 2019, 3,054 people were admitted, most with severe underlying chronic and non-communicable diseases. We assisted the hospital by improving the quality of care through early identification and monitoring of severe cases. We also opened an outpatient clinic for closer follow-up of unstable/very sick patients after they are discharged from the inpatient wards.
Advanced HIV care
In Homa Bay, we continued to work on improving HIV care and reducing transmission and mortality rates. We finalised a study to assess the results of the new approaches implemented in our HIV activities in Ndhiwa subcounty between 2014 and 2018. The programme, aimed at reducing new infections through treatment as a prevention strategy, is based on the idea that an HIV-positive person whose viral load is suppressed by effective treatment is unable to transmit the virus to others. We tested as many people as possible, put all HIV-positive patients on treatment and worked on the quality and continuity of care to help them achieve viral suppression.
The study was completed in early 2019 and showed promising results. The findings are due to be published in 2020.
In 2019, we supported HIV services in 30 government health facilities. We focused on improving the holistic management and follow-up of advanced HIV patients, paediatric and adolescent care, and management of patients on second- and third-line antiretroviral therapy (ARV), as well as ARV treatment failure.
Care for people who use drugs
Many people who use drugs in Kiambu county had to travel to the capital, Nairobi, for opioid substitution treatment, as there were no medically assisted therapy clinics locally. They often had to visit several other facilities to obtain medical care and psychosocial support.
In September, we opened a clinic in Kiambu, offering a one-stop-service centre for drug users, comprising opioid substitution therapy, treatment for HIV, TB, hepatitis C and non-communicable diseases, wound care, mental health support and counselling, and sexual and reproductive healthcare.

Care for victims of violence
MSF runs a trauma room in Mathare, Nairobi, to treat victims of urban violence in the city’s Eastlands area. The clinic is supported through a 24-hour, toll-free call centre and an ambulance programme that offers emergency care to patients and refers them for further treatment when necessary.
We also run a clinic providing specialised care for victims of sexual and gender-based violence in Eastlands, in addition to supporting Ministry of Health facilities. Services include medical consultations, treatment to prevent the transmission of HIV and sexually transmitted infections, pregnancy tests, swabs for legal purposes, psychological counselling and referrals for social and legal support. In 2019, our teams treated over 260 patients each month.
Medical care for refugees
We continue to support a 100-bed hospital and two health posts in Dagahaley camp in Dadaab. Our health services benefit not only refugees, many of whom have been in the camp for close to 30 years, but also local communities. Our comprehensive general and specialist healthcare programme in Dagahaley includes sexual and reproductive healthcare, emergency obstetric surgery, medical and psychological assistance to victims of sexual and gender-based violence, and psychosocial counselling. We also offer home-based insulin treatment, palliative care and specialist referrals. In 2019, we conducted more than 210,000 outpatient consultations, admitted close to 10,000 patients for care and assisted over 2,800 births.
Comprehensive obstetric care in Likoni
In Likoni subcounty, Mombasa, we support the Department of Health to provide comprehensive emergency obstetric and neonatal care in the fully renovated Mrima health centre. Our teams there assist an average of 6,000 births every year, perform lifesaving obstetric surgery and support ante- and postnatal care, as well as screening for cervical cancer, HIV and other sexually transmitted diseases.
Responding to medical emergencies
The high incidence of snakebites in Baringo county, northwestern Kenya, has been largely under-reported due to a lack of appropriate monitoring tools. For three months, an MSF team trained medical staff in prevention strategies and administering antivenoms and first aid to snakebite victims. We also donated antivenom vials to boost the county’s supplies.
In addition, we responded to malaria outbreaks in Baringo and neighbouring Turkana county. In September, more than 45,000 people tested positive for malaria, in the worst outbreak in Turkana since 2017.
Heavy rains later in the year led to flooding and displacement in some parts of the country. In West Pokot county, when flooding and landslides forced many people to flee their homes, we donated medical supplies and treated mosquito nets. We also provided emergency relief items and food to the most affected refugees in Dagahaley camp.