- Oxygen is the most critical medicine for people with severe COVID-19, yet its supplies are unstable in many countries.
- People in low- and middle-income countries are last in line for both preventive COVID-19 vaccines and stable medical oxygen supplies – leaving people to get sick and die.
- Governments must invest in stable oxygen supply chains, including providing more concentrators, and regulating the price of oxygen.
Brussels – Along with COVID-19 vaccines and personal protective equipment, stable supplies of medical oxygen are desperately needed to respond to the pandemic. In a briefing paper released today, titled Gasping For Air, Médecins Sans Frontières (MSF) highlights the importance of having medical oxygen supplies at the heart of the COVID-19 response. With COVID-19 vaccines unavailable in wide range of countries worldwide, people are continuing to fall ill with the new coronavirus. Without a significant investment in oxygen infrastructure, those whose illness is severe and who cannot access oxygen will die.
“Oxygen is the single most important medicine for severe and critical COVID-19 patients,” says Dr Marc Biot, MSF Director of Operations. “Yet oxygen supply is often insufficient because infrastructure has been neglected in lower- and middle-income countries for decades.”
“Before the pandemic, we saw patients suffering from pneumonia, malaria, sepsis, and a variety of other conditions, as well as far too many premature babies, die due to a lack of medical oxygen,” Dr Biot continues. “But COVID-19 has brought this issue into a sharp new focus. Unstable oxygen supplies kill.”

In the under-resourced countries where MSF teams work, hospitals and health centres often rely on unstable and expensive oxygen supply chains. Whilst hospitals in wealthy countries have their own oxygen plants and pipe highly concentrated oxygen to the bedside, patients across lower- and middle-income countries must rely on bulky, expensive and easily depleted oxygen cylinders or small oxygen concentrators which are not enough for a critical patient.
“People are being failed twice,” says Dr Biot. “Not only are they at the bottom of the inequitable global vaccine queue, but they also cannot receive care when they fall ill because they do not have access to the oxygen they need.”
Beyond the current catastrophe in India, the city of Aden, in Yemen, is another prime example of the global oxygen shortage. The MSF-supported hospital was more than completely occupied in recent days and has been going through 600 oxygen cylinders per day, whilst still having to turn away patients at the door.
Oxygen is the single most important medicine for severe and critical COVID-19 patients... yet oxygen supply is often insufficient... Unstable oxygen supplies kill.Dr Marc Biot, MSF directors of operations
“Numbers are stabilising now, but we know there will be another surge and there will be very sick patients who will need more oxygen than we can provide,” says Dr Biot. “As a doctor, it’s very distressing to see that, wave after wave of COVID-19, countries remain unprepared and medical teams are left without the essential medicines they need to save lives on the massive scale required.”
Our teams that are working in under-resourced countries are implementing creative solutions to get their patients the oxygen they so desperately need. In South Africa, oxygen concentratorsSmall machines that take the oxygen from the air but are not powerful enough to provide the oxygen needs for a critically ill COVID-19 patient. were linked together to increase their capacity. In the Democratic Republic of Congo oxygen cylinders were connected together to create a central oxygen bank.
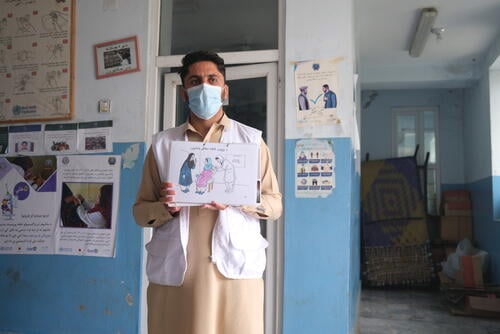
Health workers are being trained in the appropriate use of oxygen therapy. In some contexts, the prices of oxygen have been regulated to ensure that the cost does not become an unnecessary barrier as demand increases.

“Today, we don’t have the luxury of time. These kinds of practical solutions save lives and we need to see more of them,” says Dr Biot. “More concentrators must be provided, especially in rural areas where there are no oxygen plants; the price of oxygen must be regulated; and buffer stocks and reliable supply chains for facilities that rely on cylinders from existing oxygen plants must be created and maintained.”
“These steps are needed to save lives while we wait for governments to address the structural underinvestment in oxygen infrastructure that result in some patients gasping for air.”