In Pakistan, one baby in every 22 dies during its first month of life. This is the world’s highest rate of newborn mortality and a distressing statistic to which stillborn babies must be added.
Médecins Sans Frontières (MSF) provides maternal and child healthcare services in Peshawar, Khyber Pakhtunkhwa province, near the Afghanistan border, as well as in Quetta, Chaman, Timergara and the districts of Jaffarabad and Naseerabad.
Since its opening in 2011, over 25,000 women have given birth in Peshawar women’s hospital.
“Newborn mortality in Pakistan is primarily due to premature birth, complications during pregnancy and labour and infections,” explains Dr Khadija, a paediatrician in the neonatal care unit of Peshawar women’s hospital.
While the causes of death can be explained medically, they often stem from the complex and sometimes challenging social and cultural reality faced by women living in this region of Pakistan.
Most of MSF’s patients in Peshawar come from impoverished outlying rural communities where healthcare is still scarcely available, due to issues not only of cost but also access.
Other women are refugees, mainly from Afghanistan, or have been internally displaced from former Federally Administered Tribal Areas (FATA), which until the beginning of 2017 endured conflicts and instability resulting from the 2001 war in Afghanistan.
This is why care at the MSF hospital, and transport to the facility, are provided entirely free of charge. Whoever they are, all these women live in harsh and unsanitary conditions that affect their health and their pregnancies.
Fighting newborn mortality at Peshawar women's hospital
The tragedy is that a lot of women give birth in their homes without a medical professional.Dr Khadija, a paediatrician in the neonatal care unit of Peshawar women’s hospital
“To give birth to a healthy baby, the mother needs to be in good health,” states Dr Khadija. “If the mother’s nutritional status isn’t satisfactory, she’ll be unable to provide the nutrients her baby needs. For example, she won’t be able to produce enough milk and her baby’s health will suffer.”
Many women have had neither health education nor schooling. “None of us here really know how old we are. It’s a question we never ask. Most of us haven’t been to school so our age isn’t an issue,” explains Shaheen who thinks she’s 25. She’s just given birth by caesarean section, to her fourth child in as many years.
Mothers at Peshawar women’s hospital are given advice on the importance of vaccination, postnatal care, skin-to-skin contact immediately after birth and breast-feeding — all quite uncommon but so crucial to improving their babies’ chances of survival and development.
“We knew nothing about all this!” Shaheen says, speaking for herself and the other young mums who have come to participate in the discussion. They agree. “It’s wonderful, we love the contact with our babies. We’ll do it again when we have another baby!”

The importance of outreach work and medical supervision
It is still common for women in Pakistan to deliver their babies at home — in poor conditions of hygiene and without the assistance of health professionals. “There are often no drugs, no clean water and no electricity,” says Dr Khadija. The practice is responsible for the deaths of many children and mothers.
Women give birth at home because “it’s the tradition [and] everybody expects mothers to have their babies at home,” explains 35-year-old Bismilla*, who lives in a displaced people camp in Peshawar. Razmina says it’s “because the health centres are too far away from [her] village” that she gave birth to her first three children at home. Amira’s* mother-in-law adds, “I had my seven children at home and it wasn’t a bad experience.”
However, it is a proven fact that chances of survival increase significantly when labour and birth are attended by a health professional in a specialist medical facility.
Many deaths are due to complications that could so easily be avoidedDr Khadija, a paediatrician in the neonatal care unit of Peshawar women’s hospital
At the MSF hospital in Peshawar, a team of almost 100 medical staff (paediatricians, midwives, gynaecologists and nurses) work together to provide mothers and babies with the best possible care.
With its neonatal unit that has incubators, cardiovascular, respiratory and phototherapy equipment, and intravenous solutions, the hospital is still somewhat unusual in Pakistan.
Outreach health workers at the hospital advise women and those accompanying them. They also visit rural communities to inform people about the importance of getting medical supervision in primary health centres during pregnancy, as well as delivering their babies in health facilities that have the necessary equipment to provide the appropriate care.
MSF works in partnership with 32 basic health centres where mothers-to-be are monitored and then referred to Peshawar women’s hospital to give birth.
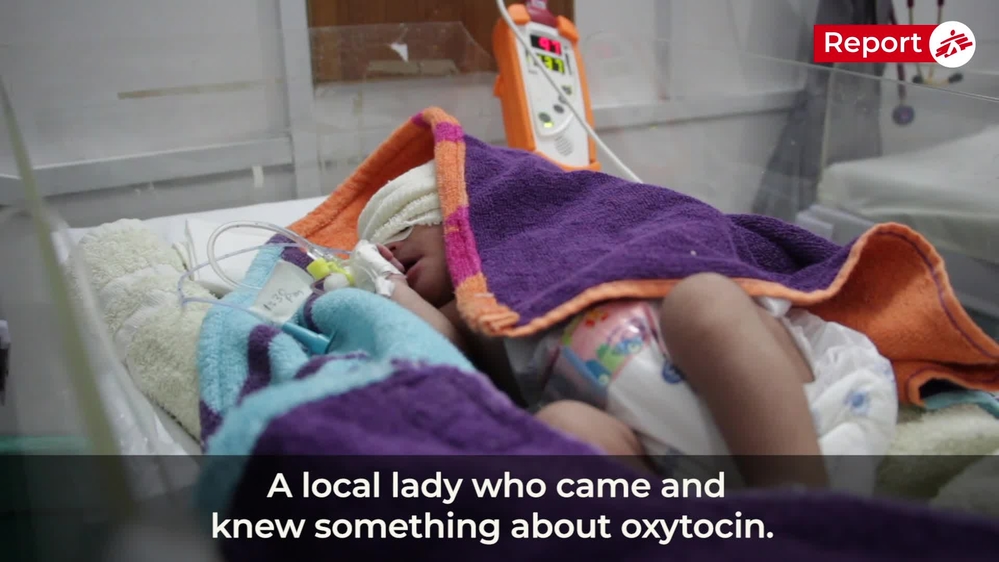
Frequent misuse of oxytocin increases the risk of death among newborns
Common in Pakistan, the oxytocin hormone is yet another cause of unsafe deliveries and contributor to the highest newborn mortality rate in the world. Freely available for less than 10 rupees (6 euro cents), it is used to stimulate contractions and induce labour.
When not administered by a skilled medical professional, oxytocin can be extremely dangerous for both mother and child. However, many women take it, often ending up with severe haemorrhaging and ruptured uteruses while their babies have breathing difficulties and some even die.
Lots of women arrive at MSF’s hospital in Peshawar suffering the effects of oxytocin, but despite the medical staff’s expertise and the equipment available to them, these cases are still extremely challenging and many babies cannot be saved.
"Just yesterday we admitted a woman who was expecting twins,” says Dr Khadija. “The mother had begun to have mild contractions so her family called in a woman from the village who gave her three oxytocin injections to speed up labour. It happens a lot. The contractions triggered by the injections were so severe that after a while she couldn’t feel one of the twins moving anymore. That was when her family brought her to the MSF hospital. We were able to save one of the twins but the other one was dead in her uterus.” Farzana, the twins’ mother, had already lost two children, one within days after its birth and one at the age of five years.
During their outreach sessions in villages and at hospital bedsides, MSF teams inform people of the serious risks they expose themselves to when the hormone is not administered properly. “Many deaths are due to complications that could so easily be avoided,” explains Dr Khadija.
In addition to providing professional medical care, MSF plays a vital role in health education and monitoring expectant mothers. Razmina is in no doubt. Whereas her first three babies were born at home, she says the next ones won’t be. “It’s more hygienic here and our children can get vaccinated.
Bismilla*, who’s just had her eighth child and wants to have more, adds, “I’ve always had my babies at home and if I hadn’t had complications during this pregnancy that’s where I’d have had this one too. But I see things differently now. There’s better hygiene here and the medical personnel are kind and always available.”
For my next children I think I would like to come back here instead of delivering in my house.Bismilla*
PATIENT STORIES

Shakeela, 48
Shakeela comes from a small village, three hours from Peshawar. Like most patients at the MSF women’s hospital, she belongs to a rural community that is still often excluded from the healthcare system and usually prefers to give birth at home. In total, she has been pregnant 17 times, but four of her children have passed away. She was 13 when she gave birth to her first child and still lives with seven of them.
On 12 September she arrived at the hospital to give birth to her 13th child. When she arrived, her blood pressure was very high, following an injection of drugs she had taken at home to speed up the delivery. Although this is risky both for the mother and the baby, it is still a very common practice in Pakistan.
Her baby was born with meningitis and had to be treated with antibiotics at hospital for 14 days until he recovered. His mother stayed with him the whole time in one of the rooms provided by MSF. It is the custom in this part of Pakistan not to name a baby when they are born, but when they return home. After two weeks in the hospital the baby was finally named: Muza Milshah.
“I am happy that my son was born safe, but now I don’t want any more babies. All my children were born as big as this one and I am now too weak. I am only living with my sons, all the girls are married… and the men, you know, they don’t do anything at home!”

Bismilla*, 35
Bismilla is from Bajaur Agency, a former district of Federally Administered Tribal Areas (FATA). She had to leave her village with her family 10 years ago due to the instability in the region resulting from the 2001 war in the neighbouring Afghanistan. She already had an 18-month-old son, when the family decided to move to Peshawar. The trip that they took on public transport was long and hard for both Bismilla and her young baby. Since the family did not know anyone in Peshawar, they settled in a camp for internally displaced people and this is where they still live now.
The young boy she gave birth to in Peshawar women’s hospital is her eighth child. The others, she delivered at home in the camp. “I wanted to deliver in my house of course, this is the tradition and everybody was expecting me to deliver at home. And everything went well, I was totally fine!”
This is what she was planning to do for this one as well, but then she started to feel severe pain. There is a small government-run hospital in the camp, but on the way there, the taxi driver advised Bismilla to go to the MSF women’s hospital instead. This is how she arrived here. “The staff are really nice and caring here, and they are always available. For my next children I think I would like to come back here instead of delivering in my house.”
Bismilla would like to have up to seven more children and refused the offer of family planning from MSF. Her husband also still wants her to have more children.
Following the local tradition Bismilla’s new baby delivered in hospital has not been given a name yet; his name will be chosen by her father. Bismilla hopes he will agree to name him Arshad.

Fatma, 23
Fatma is originally from North Waziristan, a Pakistani region on the border with Afghanistan. On 3 October she gave birth for the first time. Her baby is a girl and she feels happy and blessed. Both she and her husband hoped they would have a girl. They already had a girl’s name chosen for a long time: Anaya.
Fatma belongs to a big family, with many sisters, but only one brother. Fatma’s family knew about the MSF women hospital because some other female family members had given birth here and were very happy with the care they received. Since her husband works in Turkey, she came here with her mother-in-law.
“This is a nice hospital; it is clean and the care is good, both for the mothers and the attendants. Fatma is my second daughter-in-law to come here and I will keep coming with the others,” her mother-in-law said. It is traditional for women to go to the maternity ward with their mothers-in-law rather than their own mothers.
Fatma had to leave her region of North Waziristan four years ago because of the instability and conflicts in the region. “It was a beautiful place and I miss it. I hope that everything will calm down soon and that I will be able to go back to live there with my daughter.”
*Names changed to protect patient identity.










