Since the escalation of the war in Ukraine in February 2022, there has been a dramatic increase in the number of people with long-term injuries requiring complex care in Ukraine. These include people with blast injuries, shrapnel wounds and limb amputations, all of whom require intensive, specialised care. Some 300,000 people have been registered as living with physical disabilities, according to Ukraine’s Ministry of Social Policy, since the escalation.https://www.ukrinform.ua/rubric-society/3763345-v-ukraini-nalicuetsa-3-miljoni-ludej-z-invalidnistu-zolnovic.html?fbclid=IwAR10hQsNP_wKrm3BgQBJHmsChSlRirnvSMHxw5gnkpiwERS71xYrQT0Yaxg
The increased demand for early rehabilitation services has put extra strain on the country’s healthcare system. In response, Médecins Sans Frontières (MSF) launched an early rehabilitation project at Cherkasy hospital, in central Ukraine, in March 2023. The project integrates physiotherapy, psychological support, and nursing care to address the complex needs of war-wounded patients early in their recovery process.
‘All injuries take time’ is a sentiment that resonates deeply for both medical staff and patients at Cherkasy hospital, and for each group it holds a special meaning. For physiotherapists, it points to the significance of each minute spent on exercises and techniques immediately after surgery. For psychologists, it emphasises the value of timely counselling sessions and emotional support. For patients, it alludes to the fact that the healing process, both physical and emotional, is a journey that requires time and resilience.

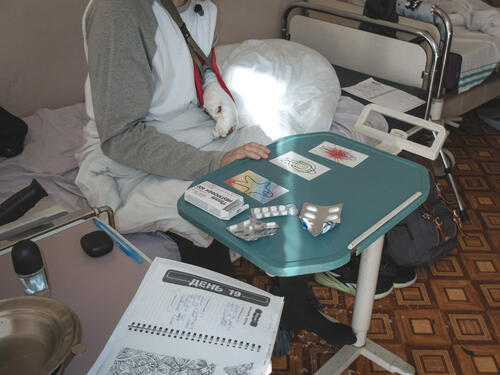
Ihor, 27, has been receiving medical treatment for over a month after sustaining multiple injuries from shelling in the Sumy region. His wounds include small fragments of shrapnel embedded in his eyes and a fractured wrist.
“At night, the pain is unbearable,” says Ihor. “I’ve screamed from the pain and even asked them to amputate my arm.”
MSF physiotherapist Oleksii Taranenko has been using therapeutic exercises and electrotherapy to treat Ihor’s injured arm, and slowly his condition is improving.
“Last night was the first time in a week that I slept through the night,” says Ihor. Over recent weeks, he has regained some ability to move his hand and can now grip a one-litre bottle of water for a short period of time.
Those few moments when he could hold something without sharp pain, with a sense of confidence, were a true achievement, and we celebrated it.Oleksii Taranenko, MSF physiotherapist
“Those few moments when he could hold something without sharp pain, with a sense of confidence, were a true achievement, and we celebrated it,” says Taranenko. “We show patients that they are capable of improvement; it’s a powerful driver for recovery.”
Many of the injuries treated in Cherkasy hospital are blast-related, and the number of patients with limb amputations is on the rise.
“Patients come with severe leg injuries from stepping on landmines or with shrapnel injuries,” says Blanche Daillet, MSF physiotherapy activity manager. “The war has created a ‘physical trauma epidemic’.”
When patients reach MSF’s early rehabilitation department, often they have been treated at two or three hospitals already. In addition to the patients’ primary injuries, MSF staff frequently encounter complications like muscle atrophy and joint stiffness. This is because surgeons often prioritise tissue integrity and the wound-healing process, which can take the focus away from restoring functionality to limbs, despite this being necessary for patients’ effective rehabilitation.

“Imagine caring for patients who have undergone 20, 30 or even 40 surgeries in a short time span,” says Vitalii Pavlieiev, MSF mental health supervisor. “These patients need support from nurses and psychologists. One patient was being prepared for a leg amputation, which the surgeons could not avoid. Our psychologists worked with him to help him accept the procedure. After the surgery, we shifted our focus to managing phantom pain.”
Sleep disorders, panic attacks and pain syndromes – particularly phantom pain following amputation – are common among MSF's patients.
Volodymyr, 42, arrived at Cherkasy hospital with leg and arm injuries. One of his fingers had to be amputated. He was also experiencing severe anxiety, disturbed sleep, and nightmares. As a guitarist and sound engineer, the amputation of his finger affected him deeply.
“I used to express everything in my soul through my fingers, but now I can’t play,” says Volodymyr. “Psychologists are people I can tell everything to – they listen to my pain.”
Patients’ mindsets and the support they receive from family and friends all play a critical part in their successful recovery, according to MSF’s mental health team. As well as providing patients with one-to-one psychological support, the team also conduct group sessions and work with patients’ families.
Through early rehabilitation, MSF aims to improve patients' quality of life, stabilise their emotional state, reduce pain, and prevent the long-term complications frequently associated with severe injuries, including the risks of infection and muscle atrophy. Ultimately, this approach supports patients in regaining independence, enabling those with severe injuries to care for themselves.
Despite the clear advantages of a multidisciplinary approach to rehabilitative care, implementing it within Ukrainian hospitals is challenging. Currently, too few staff are qualified in the relevant fields. But this is likely to change in the coming years, according to MSF emergency coordinator Thomas Marchese.
“Although more students are now pursuing relevant studies, it will take another three to four years before they enter the workforce in fields such as physiotherapy, occupational therapy, and clinical psychology,” says Marchese.
To tackle the large gap between people’s high needs and the limited numbers of qualified staff, MSF suggests making the best use of the resources available and trying to reach as many patients as possible. MSF is working closely with the Ukrainian Ministry of Health and other partners to expand its approach in Cherkasy to more regions, with the aim of lessening the lasting impact of war injuries on people across Ukraine.






