“Spending our lives in the camps is difficult; the area is small and there is no space for the children to play,” says Abu Siddik. He lives in one of the camps in the Cox’s Bazar district of southeastern Bangladesh, where around 860,000 Rohingya refugees are crammed into just 26 square kilometres of land.
“I left Myanmar because my house was burnt down. They were killing and torturing everyone, and harassing our women. It was not safe.”
Siddik is referring to the ‘clearance operations’ launched by Myanmar’s security forces which began in August 2017. They drove more than 700,000 Rohingya from Rakhine state over the border into Bangladesh. These refugees joined 200,000 others who had fled previous waves of violence.
Before escaping many experienced or witnessed horrific violence. Their friends and family members were killed, and their homes were destroyed.
Rohingya refugees in Bangladesh: three years after
Little hope for the future
Three years on there is little hope of positive change for the Rohingya, or for their returning home in a safe and dignified manner any time soon. People continue to live in overcrowded, flimsy shelters made of plastic and bamboo.
The mental health needs of the Rohingya have evolved over the years. Unemployment, anxiety about the future, poor living conditions, and little or no access to basic services, such as formal education, have added to the traumatic memories of the violence suffered in Myanmar. Some patients are receiving psychiatric treatment for severe mental health issues, including bipolar disorder and schizophrenia. Médecins Sans Frontières (MSF) teams have seen an increasing number of people with mental health issues in our facilities across Cox’s Bazar.

Poor living conditions are the main cause of disease
“The majority of the patients we see, both children and adults, come with respiratory infections, diarrheal diseases and skin infections. These illnesses are mostly related to the poor living conditions,” explains Tarikul Islam, MSF’s medical team leader in the Kutupalong-Balukhali megacamp, the largest refugee camp in the world.
There is more order now in the camps than in the early days of the emergency, with better roads and more latrines and clean water points, although access still remains extremely limited. But life here is precarious. Every year when the monsoon season arrives, the risk of floods, mudslides and losing what few possessions people have is very real.
There are also economic woes to contend with. So, it comes as no surprise then that people take their time to seek healthcare, which worsens their situation.
“Some patients arrive late, when they are already seriously ill. When a patient does not come quickly, when their condition is already complicated, and the disease is already damaging other organs in their body, it requires a lot more attention and is complicated for us to repair the situation,” says paediatrician Ferdyoli Porcel.
Back in Myanmar, many Rohingya communities received poor healthcare. This has had medical consequences and has also made people less comfortable accessing healthcare in the camps. As Ferdyoli explains,
“Another problem is related to antenatal care and deliveries at home, when women have complications during homebirths or their babies are born with complications. A delivery at a hospital can respond to these complications and gives us a chance to help the baby breath if the baby is born with problems or help the mother if she is losing blood.”
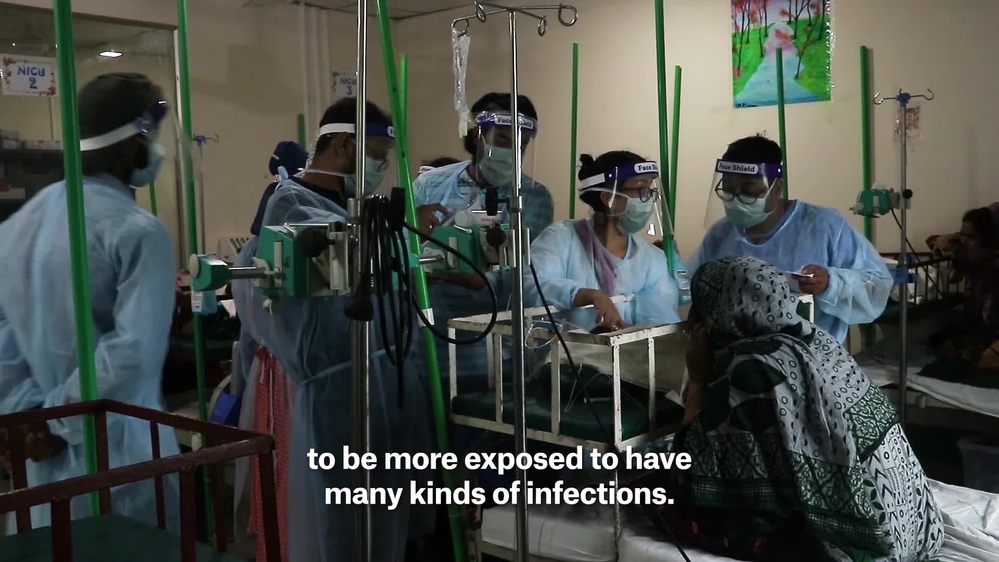
The added challenge of COVID-19
This year, COVID-19 is posing additional challenges. The first Rohingya person with COVID-19 in the camps was confirmed on 15 May. An immediate impact of this was a further erosion of trust in the healthcare system. Rumours and misinformation are rife, and fear is keeping people in need of essential non-COVID-19 healthcare away from clinics.
“Some patients were not openly admitting to COVID-19 related symptoms because they thought they would be treated differently,” says Tarikul Islam.
Jobaida gave birth a few weeks ago at the MSF Goyalmara mother and child hospital. She describes how she and her baby spent six days in the neonatal intensive care unit, during which time they were tested for COVID-19:
“The test came back positive and I was moved to the isolation ward with my baby. We spent 12 days there. I was afraid because there is a belief in our community that having COVID-19 means you will die. The doctors and nurses were really kind; they supported me and checked on me every day. They didn't seem to be afraid to get close to me, even though I was infectious, which helped me feel less stigmatised.”

Working with the communities is essential
Sharing information about COVID-19 and raising awareness among communities has been crucial to MSF’s response, but doing so using social media or SMS messaging has been hampered by restrictions on mobile network availability in and around the camps.
To avoid gathering people in groups, our outreach teams in the camps and the neighbouring Bangladeshi villages go house-to-house, speaking with individual family members.
Some healthcare providers, including MSF, had to reduce activities, particularly in the early days of the pandemic, due to staffing and resource challenges. This in turn, had consequences for those in need of medical care.
Containing the spread of COVID-19 has also meant increased restrictions on movement in the camps. This has further hampered access to healthcare and made it harder for patients with ‘invisible’ illnesses, such as psychiatric disorders or non-communicable diseases like diabetes, to prove that they are sick and to travel to medical facilities.
The situation for Rohingya refugees has been exacerbated by the COVID-19 pandemic. Their lack of legal status and the absence of longer-term and more sustainable solutions mean their future is more uncertain than ever.Alan Pereira, MSF country representative in Bangladesh
The outlook is bleak across the region
As the months and years drag on, the 25 August is a reminder of the decades of state-sanctioned violence, persecution, discrimination and denial of basic rights that the Rohingya have endured. Beyond Bangladesh, MSF sees the consequences of living in limbo for the Rohingya communities we work with in places like Myanmar and Malaysia.
The Rohingya remaining in Rakhine state continue to face discrimination and segregation, particularly restrictions on movement, which limit their access to healthcare.
In Malaysia, which hosts one of the largest populations of Rohingya outside Myanmar, many do not seek medical care or delay doing so until their condition becomes very serious for fear of being reported to the immigration authorities and detained. Barriers to accessing employment mean most cannot afford healthcare even if they want to seek it out.
Moreover, in recent months countries in south-east Asia have repeatedly refused boats carrying hundreds of refugees fleeing the camps in Bangladesh to land on their shores for fear of COVID-19. People are left adrift for weeks with little food and water and are often the victims of abuse.
“The vulnerability of the situation for Rohingya refugees has been exacerbated by the COVID-19 pandemic. Their lack of legal status and the absence of longer-term and more sustainable solutions mean that their future is more uncertain than ever,” says Alan Pereira, MSF country representative in Bangladesh.
“At a time when many around the world find their movements curtailed, their plans shelved and their livelihoods in turmoil, it is important to remember that this has been the life of the Rohingya for generations.”
MSF activities in Cox’s Bazar
In Cox’s Bazar, MSF manages 10 hospitals and primary health centres. Our activities cover a range of inpatient and outpatient services, including emergency and intensive care, paediatrics, obstetrics, sexual and reproductive healthcare, and treatment for survivors of sexual violence and patients with non-communicable diseases.
During the first six months of 2020, our teams held nearly 173,000 outpatient and emergency consultations; admitted over 9,100 patients for care; provided over 22,600 antenatal consultations; assisted more than 2,000 deliveries; and gave more than 14,250 individual mental health consultations.
In response to COVID-19, MSF teams are carrying out health promotion activities to raise awareness and educate communities. We are training frontline workers on infection prevention and control measures, and have set up isolation wards in all our health facilities and dedicated treatment centres.







