Cervical cancer accounts for 37 per cent of new cancer cases among women in Malawi. Since 2018, Médecins Sans Frontières (MSF) has been working to reduce the incidence of cervical cancer and bring down deaths related to the disease in the districts of Blantyre and Chiradzulu. Our head of mission in Malawi, Marion Péchayre, explains how.
Why did MSF turn its attention to cancer patients?
Our interest in cancer is the result of a combination of factors. In low-income countries, epidemiological projections suggest a decline in infectious diseases and a simultaneous rise in chronic diseases such as cancer.
The lack of resources and the late stages at which cancers are diagnosed in sub-Saharan Africa, for example, suggest that they will eventually claim more lives than infectious diseases, as they do currently in high-income countries. The World Health Organization (WHO) estimates that cancer mortality will double in Africa by 2040.

In Malawi, where we have been providing HIV/AIDS care for many years, we found that a lot of our patients had cervical cancer, too. Women with HIV are six times more likely to get cervical cancer. This led us to carry out a comprehensive assessment of the cervical cancer problem in Malawi, which has the second highest prevalence and mortality rates in the world.
In 2020, 4,145 new cases of cervical cancer were detected and 2,905 women died. Access to anti-cancer drugs is highly variable, radiotherapy is non-existent, and surgery is poorly developed. We are interested in supporting vaccinations to protect against cervical cancer where possible, as well as extending screening programmes and developing treatment solutions.
How do you treat cancer in the absence of radiotherapy?
Radiation therapy is normally the first-line treatment for cervical cancer, but it is not currently available in Malawi. Over the past two years, our teams have developed a model of care that combines chemotherapy and surgery.
After three to six cycles of chemotherapy, tumours shrink and can be operated on, saving patients’ lives. We don’t yet have the data to assess the two-year survival rate, but the treatment shows satisfactory results and can be expected to provide a life expectancy close to that of treatment with radiotherapy.

In resource-limited countries, this type of treatment could be considered as a serious alternative to radiotherapy, as long as there are well-trained surgeons. This is why our teams have paid particular attention to training the surgeons who perform advanced surgical procedures such as hysterectomies, where the uterus is partially or totally removed.
Each month in our project, surgeons perform an average of 14 hysterectomies, and 40 surgeries in total. As a result, these surgeons have become highly specialised and have acquired a higher level of competence in the field of gynaecological oncology surgery.
In addition, the quality of treatment is ensured by multidisciplinary work, involving anatomical pathology, oncologists, surgeons and supportive care teams, who provide social and psychological support, physiotherapy or palliative care.
In the case of women whose cases are detected at a more advanced stage, we arrange and finance referrals to Kenya so that they can have radiotherapy there. But these referrals require significant support and resources, and patients cannot benefit from them on a large scale. However, by the end of 2023, we should have access to radiotherapy in Malawi, which will make it much easier to arrange treatment for women with advanced cervical cancer.
How do vaccinations help?
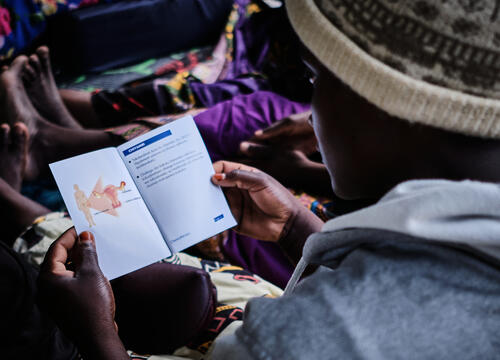
Vaccination is crucial because cervical cancer is easily preventable. It is one of the few cancers associated with a virus, the human papillomavirus (HPV), and there is an effective vaccine against some HPVs. The other way to protect against cancer is screening, which is both a means of prevention and the first phase of treatment, as pre-cancerous lesions can be treated at this stage.
The HPV vaccine is made available through international mechanisms such as GAVI, but routine vaccination in health centres does not easily reach the target population in Malawi, i.e. girls aged from nine to 13. Girls at this age don’t come to health centres as they don’t generally get sick, so they must be vaccinated either at schools or in their villages.
Such systematic prevention programmes in schools and communities require additional resources. We will continue supporting these vaccination programmes, in partnership with the Malawian Ministry of Health, as we did in January, when we vaccinated 17,000 adolescent girls in the Phalombe district.






