London - A report released by the humanitarian medical aid organization Médecins Sans Frontières (MSF) shows that major donor agencies such as the UK's Department For International Development (DFID) and the US Agency for International Development (USAID) are continuing to support cheap, but failing malaria treatment in Africa despite a rising death toll from the disease.
The new report, called "ACT Now", documents the dramatic rise in malaria in the last decades: the number of cases were four times higher in 1990s than they were in the 1970s; and death rates in African hospitals have risen two- to three-fold. The continuing use of ineffective drugs despite alarming levels of resistance is leading to increased treatment failure and deaths.
The report calls on international donors to put their weight behind rapid implementation of artemisinin-based combination therapy (ACT), a proven treatment that is being promoted by the World Health Organization (WHO).
"Since 2001 WHO experts have recommended replacing failing malaria medicines with more effective treatments, but donors have failed to encourage this change, choosing to save money rather than lives," said Dr. Bernard Pécoul, Director of MSF's Campaign for Access to Essential Medicines. "The G8 and African leaders' goal of halving malaria deaths by 2010 will remain a fantasy unless donors are willing to help pay for treatment that works."
Since 2001 WHO experts have recommended replacing failing malaria medicines with more effective treatments, but donors have failed to encourage this change, choosing to save money rather than lives"Dr. Bernard Pécoul, Director of MSF's Campaign for Access to Essential Medicines
While many African countries are heeding the malaria advice of WHO experts to adopt combination treatment protocols, a lack of domestic resources and international help are forcing countries to switch to stop-gap, less expensive combinations. But implementation of new malaria recommendations is a matter of life and death in Africa, where the disease kills between 1 and 2 million people each year. Sickness and death from malaria account for 30-50% of hospital admissions and a yearly loss of US$12 billion on the African continent. To counter the rising death toll, WHO is now recommending stepped up prevention including increased use of insecticide-treated bednets and introduction of ACT. Artemisinin drugs are highly potent, fast-acting and very well tolerated. However, donors, in particular the US and the UK, are balking at ACT introduction in Africa due primarily to its higher cost.
In 1969, when malaria eradication was abandoned, the focus of international control efforts switched to treatment. At the time, the treatment of choice was chloroquine, dispensed in a three-day course. This effective treatment campaign led to falling death rates until the early 1980s. But this drug is no longer working in most African countries. For example, in 1999 Tanzania had resistance rates from 28-97%, Kenya 66-87% and Uganda 10-80%.
Currently an adult dose costs about US$1.50 and is expected to go down to US$0.50 -0.80 in 2004-2005, while older drugs are about US$0.10. MSF has estimated that the cost of changing to ACT for all of Africa would be between US$100-200 million.
"But what would you rather do - waste money on old cheap drugs that you know don't work or fund a more expensive treatment that will save lives?" said Dr. Nick White, Professor of Tropical Medicine, Mahidol and Oxford Universities in the MSF report.
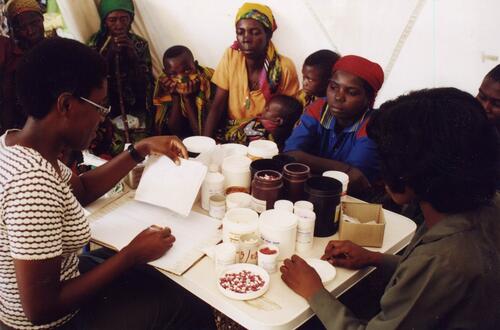
MSF uses ACT in Angola the Democratic Republic of Congo, Congo-Brazzaville, Zambia, Liberia, Kenya, Ivory Coast and South Sudan and is working to adopt ACT in all its programmes. With international help, some African countries have already changed or are in the process of changing to ACT. KwaZulu Natal province in South Africa has successfully managed to change while Burundi, Zambia, and Zanzibar in Tanzania are preparing for implementation.
"Donors need to act now because attempts to control malaria with scaled up prevention and old treatments are doomed to failure," said Pécoul.