The last in a three-part series commemorating 30 years of MSF activities in Armenia
In Armenia, MSF launched its first functional rehabilitation and limb-reconstruction projects (following the devastating wounds caused by the 1988 earthquake), it carried out advanced surgery and vital research on multi-drug resistant TB and hepatitis C.
Let us also not forget this is the first time MSF has run activities in a post-Soviet context, opening the doors to a new region and new challenges for us.
As we prepare to hand the activities over to the local health authorities, we have an opportunity to look back on a great mission and the role it played in the development of MSF as an organisation.
For MSF, Armenia has been a mission of game-changing medical and operational breakthroughs: from the very first paediatric mental health activities to pioneering the current endTB campaign, so much has been done here over the past 30 years, always with the well-being of our patients at the top of our minds.Mathilde Berthelot, MSF Armenia Desk Manager
2005: Tackling drug-resistant tuberculosis
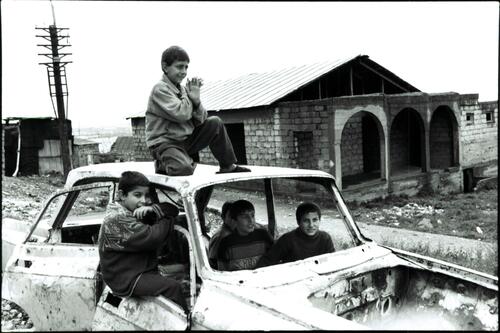
After the collapse of Soviet Union, war, poverty and weakness of health system contributed to the spread of tuberculosis (TB), in particular drug-resistant forms of the disease (DR-TB).
In 2005 the programme was reoriented specifically towards drug-resistant TB due to the reported increase of the disease and the fact that the national programme was taking its first steps in this direction.
“TB programmes saw their supplies of drugs virtually grind to a halt, and people would stop and start their treatment as they went off to war. The TB programme was no longer a priority for the community,” Maryline Bonnet, former MSF TB advisor, said in 1998.
In 2005, MSF started supporting the Armenian Ministry of Health in the Shengavid and Malatian polyclinics in Yerevan, to provide DR-TB patients with systematic access to effective drugs.
Rather than standing in for the government, MSF tries to ensure that the government has the ability to provide comprehensive and quality care to TB patients in ArmeniaAnabelle Djerbi, head of mission
Over the years, the MSF programme was gradually expanded to encompass all TB cabinets in the country.
In 2008, MSF also started supporting care for patients in the penitentiary system, considering detainees to be among the worst affected.
MSF introduced decentralised care. To improve adherence, patients would take their daily treatment in TB cabinets, supervised by nurses – in line with the directly observed TB treatment (DOTS) model of care recommended by the World Health Organization (WHO).
Multidrug-resistant TB
Multidrug-resistant TB (MDR-TB) treatment is extremely difficult for patients to follow: it lasts two years, there are many pills to take every morning, and a good adherence is needed throughout the two-year treatment, the potential side-effects of which include nausea and vomiting.
MSF provided such patients with comprehensive care to help increase their chances of success. This meant providing medication to prevent and treat the side-effects of the TB drugs, conducting laboratory tests and imaging and managing other chronic diseases, as well as providing psychological care, counselling, education and support, including financial support.
For the most severely ill patients, unable to attend TB cabinets every day to get their treatment, MSF supported home-based care, with daily visits by a nurse that served as an example for the Ministry of Health to follow it in national strategy.
Together with the Global Fund, MSF renovated the DR-TB unit in Abovyan hospital, where patients would spend the first two to four months of their treatment, until they are no longer contagious.
Extremely drug-resistant TB
In spite of MSF’s and the Ministry of Health’s efforts, there remained patients for whom there were not enough effective drugs – patients with extremely drug-resistant forms of tuberculosis (XDR-TB).
In response, MSF imported new generation anti-TB drugs bedaquline (from 2013), then delamanid (from 2015).
The development of these new TB drugs is a major achievement of the last 40 years, bringing new hope for patients with extremely resistant forms of the disease. Many patients who were on ineffective treatment for years have been cured and many lives saved.
In 2015, MSF’s project in Armenia was included in the endTB observational study, which demonstrated the efficacy and safety of these new drugs.In 2018, the WHO released new recommendations for MDR-TB treatment, including bedaquiline as a first-option drug.
Then, in 2016, MSF introduced ‘video DOT’, another innovation for Armenia. Patients on delamanid must take a second dose in the evening, but using Skype on their smartphones, nurses can connect with their patients and maintain their ‘direct observation’.

2013-2017: Surgery for TB patients
For some patients, TB drugs are not enough – they need surgery to remove the part of their lungs most affected by TB.
Thoracic surgery is not available to TB patients in Armenia, so MSF has sent surgeons to Abovyan on three separate occasions, as a result of which 15 patients have received surgery.
“I have spent seven years in hospitals because of TB. I know every single drug and its side-effects by heart,” one patient said. “Now, after MSF operated on me and I have finished my treatment, I am joyful and happy with my family, my children, my neighbours… This is the life! I’m still young, I’m 60 years old, and I’m still useful to my community, my people.”
2016: Ground-breaking treatment for TB patients co-infected with hepatitis C
In December 2016, MSF took up another challenge: that of hepatitis C among DR-TB patients, having found that 20 per cent of its DR-TB patients had chronic, active hepatitis C. This affected their liver function and worsened the side-effects of the DR-TB drugs.
MSF initiated systematic screening, diagnosis, treatment and follow-up for all DR-TB patients. Those diagnosed with hepatitis C were given new, very effective directly-acting antivirals (DAAs).
This was the first time in the world that DAAs had been administrated at the same time as DR-TB drugs.
According to the first results, 29 out of 31 co-infected patients who completed DAA treatment were cured of hepatitis C. What’s more, those who were still on DR-TB treatment could complete their TB treatment and stood a better chance of being cured of both diseases.

Fighting two diseases at once
Looking to the future
Given the immense progress made over the years, in 2016 MSF started the gradual process of handing over its activities to the Ministry of Health.
While continuing to treat patients enrolled in the endTB observational study, MSF is training and briefing Ministry of Health staff to run the other activities developed.
As part of the handover of our last project to the government’s structures, we consider that part of our mission is to make a realistic assessment of the situation and to support the Ministry of Health and other health partners in the identification of future directions.
This is a step-by-step process, the aim being for MSF to withdraw completely from Armenia in March 2019, on completion of the endTB study.