1,960,100
1,960,1
1,002,400
1,002,4
137,200
137,2

48,600
48,6
27,500
27,5
5,800
5,8

5,700
5,7
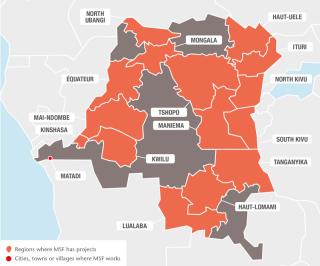
Poor infrastructure and inadequate health services continue to restrict access to medical care in the Democratic Republic of Congo (DRC). The eastern provinces remain insecure, as the Congolese army and several armed groups fight for control of resource-rich territory.
An outbreak of yellow fever hit all the provinces bordering Angola in 2016. MSF supported the Ministry of Health in a massive emergency response and vaccinated more than a million people in Kinshasa and Matadi city, Kongo Central. In Haut-Uélé province, eastern DRC, MSF also collaborated with the Ministry of Health to treat more than 84,000 patients in an exceptional outbreak of malaria. The Pool d’Urgence Congo responded to 26 emergencies relating to cholera, measles, typhoid fever and displaced people, reaching 330,000 people across the country.

North Kivu
In Walikale, Mweso, Masisi and Rutshuru, MSF continued its comprehensive medical programmes supporting the main reference hospital and peripheral health centres to provide both basic and secondary care to people affected by recurrent violence who would otherwise have little access to medical services. Almost 35,000 children suffering from malnutrition and/or other diseases were admitted to MSF-supported hospitals; over 270,000 outpatient consultations were provided in the Mweso area alone, nearly half of which were for malaria; and more than 7,500 surgical interventions were performed in Rutshuru hospital.
Between March and June, MSF responded to a nutrition emergency in three health zones in Lubero, treating over 600 severely malnourished children.
MSF continued to support five health facilities in Goma, offering screening and treatment for HIV/AIDS. In 2016, the team provided care for over 2,600 patients living with HIV/AIDS. MSF also responded to a cholera outbreak, treating more than 700 patients.
South Kivu
MSF supports two hospitals, several peripheral health centres and different community points for decentralised identification and management of malaria and malnutrition in Lulingu and Kalehe, with a particular focus on malaria and malnutrition, for children and pregnant women. Over 284,000 outpatient consultations were carried out, 10,800 people were admitted to the hospitals, more than 10,700 malnourished children were treated and more than 10,000 deliveries assisted. MSF also continued to support Shabunda and Matili hospitals.
MSF has seen a huge increase in malaria cases in recent years and the hospital it supports in Baraka is struggling to cope. A 100-bed facility built by MSF was in full use again, and more community-based sites were set up to treat 200,000 children for malaria, pneumonia and diarrhoea. Staff carried out over 450,000 outpatient consultations and admitted more than 17,000 patients to the hospital.
MSF teams continue to support health centres in Lulimba, Misisi and Lubondja. This year they opened further community-based sites and carried out nearly 200,000 outpatient consultations, including 131,322 for patients with malaria. Staff also treated 396 patients for tuberculosis (TB) and 384 patients for HIV.
Ituri, Haut-Uélé and Bas-Uélé
In early 2016, MSF opened a project to assist victims of sexual violence in Mambasa region, a mining area in Ituri where there have been recurrent attacks by armed groups and bandits. Teams provided care for over 1,100 victims of violence and treated 11,900 patients with sexually transmitted infections in nine MSF-supported health centres.
MSF continued to support Boga and Gety regional hospitals and several health centres, offering treatment for pregnant women and children, and emergency and intensive healthcare. Overall, teams treated 3,300 patients in the emergency room and intensive care unit and over 280 victims of sexual violence. More than 600 deliveries were assisted in Boga and over 2,200 children were admitted to the paediatric ward in Gety hospital.
MSF teams also responded to outbreaks of cholera and malaria, and offered assistance to displaced people. In Haut-Uélé, more than 84,000 patients were treated for malaria during an outbreak between May and August.
Tanganyika
MSF teams supported two hospitals and several health centres in Manono and Kabalo during a nutrition emergency. By late August, the Kabalo project had closed, but MSF staff continued to work in the paediatric ward in the hospital and several health centres in Manono. More than 6,000 children, suffering mainly from malnutrition and malaria, were admitted to the paediatric unit. At the end of 2016, there was an escalation in intercommunal violence and the team treated over 200 wounded patients in the hospital.
MSF also continued to work to bring cholera under control in four health areas around Kalemie. After donating a 500m3 water tank to the water authority, the project closed in March. In Nyunzu, MSF responded to a measles outbreak and vaccinated around 90,000 children.
MSF handed over its activities to the health authorities in Shamwana territory at the end of August. For 10 years, MSF had been providing comprehensive healthcare in the hospital, seven health centres and at a number of specialised community-based sites for the treatment of malaria. In the last months, 34 women were treated for vesicovaginal fistula.
North Ubangi
MSF’s project in Bili and Bossobolo continued to provide care to refugees from Central African Republic and the host communities. More than 80,000 consultations were carried out and 9,300 patients were admitted to MSF-supported hospitals.

Kinshasa
MSF offers comprehensive medical and psychosocial care for people with HIV/AIDS in the capital. Teams support several hospitals and health centres, and have been piloting innovative ways of managing patients, such as patient community groups, and providing three-month supplies of antiretrovirals. In 2016, Over 2,500 patients with advanced HIV were admitted to hospital and 68,000 consultations were carried out. Towards the end of the year, MSF supported 10 health facilities to treat 160 patients who were wounded during violent protests against President Kabila. Similar support was given to health facilities in Lubumbashi, where were 35 wounded were treated.
On 11 July 2013, four MSF staff were abducted in Kamango, in the east of the Democratic Republic of Congo, where they were carrying out a health assessment. One of them, Chantal, managed to escape in August 2014, but we are still without news of Philippe, Richard and Romy. MSF remains committed and mobilised to obtain their liberation.
3,509
3,509
109.8 M
109.8M
1981
1981
Find us online
PATIENT STORY
ELYSÉE – 18, from Ngola, South Kivu, DRC
We often have to flee clashes between the armed groups and the regular army. That’s why we can’t tend our fields. When we’re able to return, either the crops have spoiled or they’ve destroyed or burnt them all. Life is difficult in Ngola and it’s tough to find food in the forest. My three children and I received some food only once from an NGO and now my children have been treated at the Makala health centre for free. I thought I was going to lose one of them to malaria. The distribution of soap, blankets, fabric (for the women to carry children, swaddle babies and use as clothing), mosquito nets and farming tools will help us, as we have nothing ─ we have lost it all. We need everything.
Ngola, in Lulingu, is quite isolated. Only MSF was able to distribute the non-food items. They used 30 motorcycles in an operation that took more than a week.