Then and Now is the unfolding story of Médecins Sans Frontières (MSF) in Lebanon, first presented as a multimedia exhibition in Beirut on 10-13 December 2018 to commemorate the 42-year relationship between MSF and Lebanon
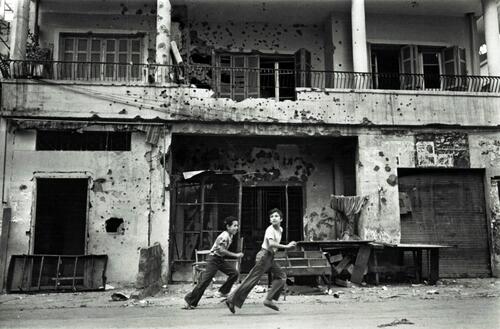
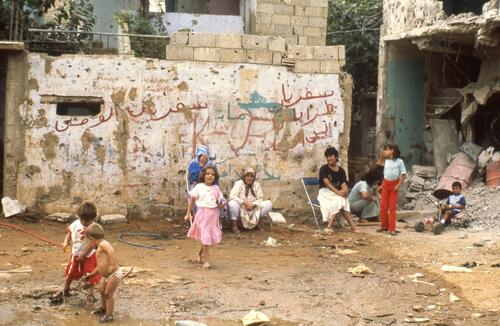
1975: Lebanese civil war erupts
A multifaceted and devastating conflict. By its end 15 years later, in 1990, over 100,000 will be dead, 17,000 missing, life expectancy will be halved, and almost 50 per cent of the population will suffer from war-induced mental health issues and trauma.
1976: MSF starts providing medical aid in Lebanon
For the first time since its founding, MSF decides to provide essential medical assistance in a war zone. An immensely risky operation to alleviate the needs of Lebanese and Palestinian communities, it will shape MSF’s activities in conflict zones for decades to come.


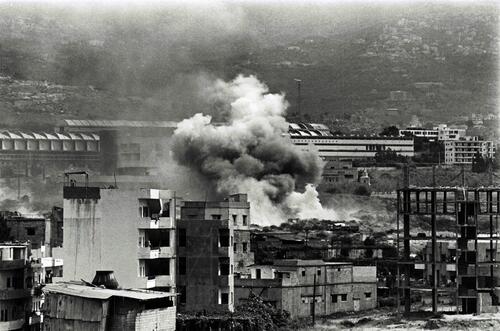
1982: Israel launches an invasion deep into Lebanon
The Israeli military reaches as far as Beirut, laying siege and indiscriminate fire on the capital and its people. Nearly 20,000 civilians are estimated to have been killed. The Israeli army will occupy Lebanon, particularly its southern region, for over two decades.


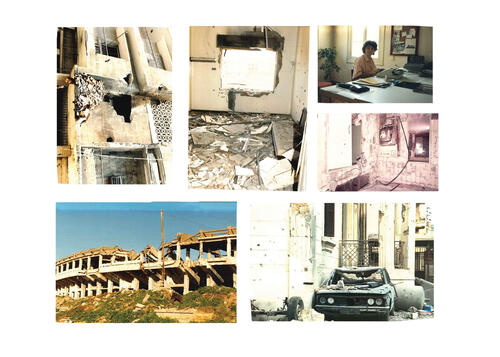
1987-1990: The Lebanese civil war enters its closing chapters
MSF teams leave Beirut in 1984, returning on an emergency basis in 1987 as the Lebanese civil war enters its closing chapters.


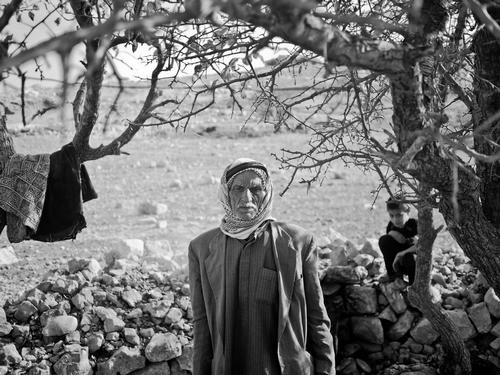
1990-2000: The Lebanese civil war officially ends
Despite the signing of the Taif Agreement in 1989, and after the guns fall silent, communities in Lebanon still face major medical needs, in additional to assistance for the traumatic experience of the Israeli occupation of southern Lebanon.
MSF teams respond to the psychosocial effects of living in such intense circumstances, launching several mental health projects especially in the south.
Facing a substantial armed resistance, the Israeli army withdrawals from most of Lebanon in the spring of 2000.

2006: The 34-day Israeli war on Lebanon
From 2000, as the Israelis withdraw from Lebanon, MSF winds down its operations in the country, focusing on mental healthcare in Palestinian refugee camps and in southern Lebanon.
But when another Israeli war on Lebanon erupts in 2006, MSF responds to the emergency by increasing medical and logistical support to the country.
In order to do this, MSF teams, working in collaboration with Greenpeace, ‘break the blockade’ on Lebanon, move supplies to the southern affected areas, and provide ongoing medical assistance to the affected population.
More than 300 tonnes of supplies are sent by sea from Cyprus to Beirut, including relief items, medical supplies, and logistical materials.
The 34-day conflict results in more than 1,100 dead, most of them civilians, over 1 million displaced and major damage to civilian infrastructure due to air strikes.



2008: MSF establishes long-term mental healthcare services
MSF decides on an initial plan to run three-year projects throughout different parts of the country, with a focus on mental healthcare.


2011: The Syrian war and its impact on Lebanon
With the outbreak of uprisings across the region, emergencies and needs intensified.
Lebanon is impacted by the Syrian war. More than a million Syrian refugees desperately escaping the violence and difficulties cross the border into Lebanon. The Lebanese medical and health infrastructure faces incredible strain.
MSF decides to rapidly expand the scale and scope of its operations to support the needs of vulnerable communities within the refugee and hosting population.
MSF projects and mobile clinics expand from Beirut to include the north (Wadi Khaled), south (Saida), and east (Bekaa) of Lebanon.
Out teams offer quality and free medical services including paediatrics, comprehensive sexual and reproductive healthcare, treatment for chronic diseases and mental health support. Activities that continue to this day.



MSF is currently present across 13 different locations in Lebanon, running primary healthcare programmes with a focus on non-communicable diseases care, sexual reproductive health and mental healthcare, in addition to three mother and child care centres. At secondary and tertiary healthcare levels, MSF provides paediatrics services and non-emergency surgeries, responding to the needs of the most vulnerable populations in Lebanon.

Non-communicable diseases (NCDs) are the biggest killer in countries like Lebanon
Chronic diseases begin out of sight, with symptoms taking years to emerge. By the time they appear in full view, they can be life-threatening without treatment.
MSF has managed an NCDs treatment programme in Lebanon since April 2012, to meet the needs of Syrian refugees, vulnerable Lebanese patients, and others who don’t have access to services or cannot afford the high cost of medical consultations, examinations, and treatment.
Today, MSF is supporting 13,700 NCD patients - the largest number of NCDs patients for MSF worldwide.
Across its clinics in Lebanon, MSF provides consultations, laboratory tests and medications for NCDs such as hypertension, diabetes (types I & II), cardiovascular disorders, asthma, and epilepsy.
Alongside this direct medical care, MSF’s health educators provide awareness and counselling sessions inside the clinics and during outreach activities to develop the patients’ understanding of their disease and improve adherence to treatment and encourage lifestyle changes to get better.
MSF’s NCD programmes in Lebanon offer innovative solutions adapted to the difficult living conditions of patients, such as home-based NCDs care, home-based Glucometer and Glucose Sensor Implant, which ensures better follow-up for complicated cases.

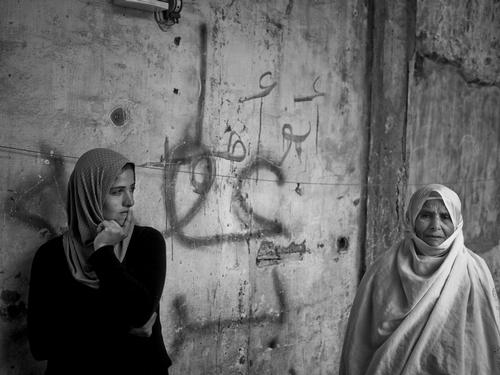
There can be no health without mental health
For vulnerable communities in Lebanon, mental health and psychological support services remain substantially unaddressed.
Since 2008, MSF provides free mental health counselling through transversal services in its primary healthcare clinics across Lebanon.
Complementing its targeted psychosocial support, MSF organises support groups and its mental health counsellors participate in outreach activities within communities.
Working alongside the community, counsellors can detect and refer those in need of mental health support. The earlier help is sought, the more the impact of mental disorders can be mitigated.
In rural areas of Lebanon, where access to psychotherapy and specialised mental healthcare is virtually non-existent, MSF implements the World Health Organization’s Mental Health Gap Action Programme (MHGAP), an initiative propelled by the Lebanese Ministry of Public Health to address large gaps within psychiatric services for vulnerable populations.
Through MHGAP, general practitioners are trained to provide – under the supervision of an external psychiatrist – medical support for substance abuse, psychotic and neurological disorders in areas where vulnerable individuals and communities have little or no access to quality psychiatric care.

Syrian Refugees in Lebanon: Coping is not an easy task - ENGLISH Version

Almost 99 per cent of female fatalities during childbirth or from pregnancy-related complications in developing countries.
Most of these deaths can be prevented.
MSF identified access to affordable sexual reproductive health services (SRH) and free-of-charge deliveries as a particular need among refugees and vulnerable communities in Lebanon.
To ensure healthy pregnancies and safe deliveries, MSF integrated SRH services into its primary healthcare package across its clinics. The SRH services include antenatal care, postnatal care and family planning with a community approach to spread awareness about family planning methods.
MSF also runs a mother and child care programme in three locations: Arsal, Majdal Anjar and Beirut. The programme is based on a midwifery-led model, in which non-complicated deliveries (normal vaginal deliveries) and newborn care are performed at the clinic, while complicated cases are referred to partner hospitals.
In May 2018, the Rafik Hariri University Hospital (RHUH) signed a memorandum of understanding with MSF in Lebanon, in which MSF will run a birth centre at the RHUH campus under a three-year renewable agreement. RHUH and MSF agreed to combine their capacities, with emphasis on the importance and relevance of the midwifery model of care.

In humanitarian settings, children are the most vulnerable, with the highest risk of disease and mortality
60 per cent of all MSF patients worldwide are children
In the Bekaa Valley of eastern Lebanon, there are around 500,000 Syrian refugees, and most of them are women and children.
The Bekaa Valley faces a lack of access for both vulnerable Lebanese and refugee communities to affordable secondary and tertiary healthcare services, and those that do exist are private and very costly.
Since March 2017, MSF provides comprehensive paediatrics care (inpatient and outpatient) to vulnerable populations, in collaboration and partnership with the Lebanese Ministry of Public Health (in Elias Haroui Governmental Hospital) and the medical NGO, Women and Health Alliance International (WAHA).
MSF's activities are an integral part of Elias Hraoui Governmental Hospital, a massive hospital with extensive and immediately available support services. MSF's service has a capacity of 28 beds that provides paediatrics care. At ambulatory level, the objective of the partnership with WAHA is to guarantee a continuum of care for patients suffering from acute and chronic complex conditions.
Through its paediatrics programme in Zahle, MSF provides specialised and free healthcare, including intensive care unit and Thalassemia care services.



