On April 13, 1994, Dr. Jean-Hervé Bradol, MSF’s Rwanda and Burundi program manager, arrived in Kigali with his emergency team to open a surgical program and treat survivors. Twenty years later, he pays tribute to hundreds of murdered Rwandan MSF colleagues.
The day after we arrived, we went with the ICRC medical team to the main hospital in Kigali, where we had arranged to work. When we got there, we and the ICRC medical coordinator realised immediately, that that would be impossible because wounded patients, particularly Tutsis, were being killed. So we decided to work with the ICRC to set up a field hospital on private land, occupied by a religious centre, adjoining the site where the ICRC delegation was housed.
The head of the ICRC delegation and his deputies took charge of obtaining permission from the interim government – the government responsible for the genocide, so to speak. Another team built the field hospital from the ground up and got it running. A third team, which I was part of, went out into the city in the morning to pick up wounded patients from organisations that were still providing shelter to Tutsis or government opponents.
Most of those sites were religious institutions where people had gathered, hoping to be protected, which was absolutely not the case. The militias and soldiers generally managed to get in and grab some of the people who had taken refuge there to kill them.
They told us that our work was pointless because they were going to kill all the Tutsis anyway.Jean-Hervé Bradol, MSF’s Rwanda and Burundi program manager
Patients could not leave the hospital
When we got to the militias’ barricades, they told us that our work was pointless because they were going to kill all the Tutsis anyway. In practical terms, it was impossible to transport adult men. We sometimes managed to transport women and children, although we couldn’t always be sure of succeeding. On April 14, Rwandan Red Cross colleagues saw militia fighters take wounded patients out of ambulances and kill them on the side of the road.
My job was to triage the wounded. Since it was dangerous to transport patients, we had to identify people who needed lifesaving surgery. I examined each wounded patient and tried to determine whether it was worth the risk of travelling through part of the city and crossing all the militias’ barricades. We treated less serious wounds on site, knowing that medical care was less critical to those patients than avoiding militia fighters who were planning to kill them.
Unfortunately, it took us several days to realise that patients could absolutely not leave the hospital and go back into the city for fear of their lives. So we organised and requisitioned neighbouring houses to expand our capacity for wounded patients who had received treatment, even when they could have gone back home.
Sites of refuge turned into slaughterhouses
We all expected killings after the president was assassinated – that was obvious to everyone. There was absolutely no progress on the political negotiations and implementation of the Arusha accords. So everyone expected a huge outbreak of violence, with lots of wounded non-combatants, and particularly Tutsis. But the events were upsetting, it all happened very quickly, and we really felt like we were running to keep up and try to understand what was happening.
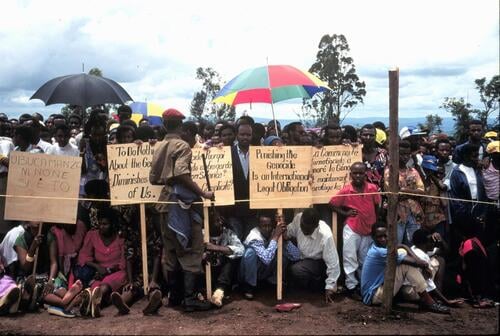
Another problem we had to face was the misappropriation of aid for criminal purposes – to kill people. That was obvious during the genocide. Sites of refuge turned into slaughterhouses. Hospitals and religious centres, places where people would normally be welcomed and protected, were, instead, primary execution sites. People gathered there, deceived by the notion that these churches or hospitals could protect them. That misperception persisted throughout the years of the conflict.
In Zaire, after the Rwandan Patriotic Front’s July 1994 victory, those who committed genocide controlled the refugee camps and diverted large quantities of the food intended for refugees to sell to Tanzanian or Congolese merchants. That money allowed them to reconstitute their forces and resume their assault in Rwanda.
We faced our own limits
We also faced our own limits. There were large-scale dysentery epidemics in the displaced persons and refugee camps but there was no generic form of the antibiotic we needed. The drug was much too expensive for humanitarian organisations and our efforts to combat the illness were ineffective. And we didn’t have the specialised food for children that we have today, so severely malnourished children recovered much less quickly and often abandoned treatment.
The Rwandan crisis was the starting point for a critical analysis of the performance of humanitarian organisations. It constituted a second wave in the professionalisation of contemporary humanitarianism. We were all forced to confront these questions because the scale of the intervention, the large number of deaths and the severity of the situations placed us face-to-face with our own technical powerlessness.
I look back with a profound sadness
I am left with a great sadness because we lost a huge number of colleagues. We don’t know the exact number. Our offices were looted and our personnel lists were destroyed so it was impossible to get a precise count. However, we believe that at least 200 of our Rwandan colleagues were killed during the genocide. I still think that we could have done a better job to try to help them flee. We were so surprised by the breadth and radical nature of the events that we didn’t always do what was necessary as an institution to help our colleagues. I look back with a profound sadness.