589,100
589,1
173,200
173,2
86,300
86,3

59,500
59,5
42,300
42,3
10,500
10,5
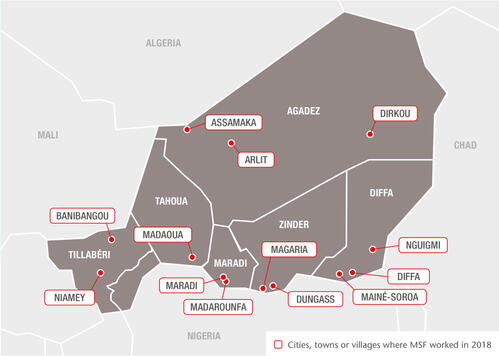
As well as paediatric care, in 2018 we also responded to disease outbreaks and helped improve vaccination coverage in Niger, while increasing the assistance we provide to victims of violence and displacement, migrants and host communities.
Responding to emergencies
We continued to support the health services with vaccinations, epidemiological surveillance and emergency interventions to tackle disease outbreaks across Niger. To curb meningitis and measles epidemics in Tahoua and Agadez regions, we vaccinated almost 262,000 people.
Between July and October, we treated over 2,500 patients during a cholera epidemic in Maradi and Tahoua regions. When the outbreak began to ebb, we supported the preventive vaccination of 167,000 people in high-risk areas.
In addition, our emergency teams distributed relief kits to over 5,000 people displaced by flooding or violence in Niamey, Tillabéri, Agadez, Tahoua and Diffa. They also provided mental health support to 423 individuals, to help them overcome the trauma they experienced.
Diffa region
After four years of armed conflict, 250,000 refugees and internally displaced people are still living in dire conditions in Diffa’s informal camps. Insecurity and a lack of resources have also had a devastating impact on local communities.
In 2018, our teams worked in the main maternal and paediatric hospital in Diffa town, the district hospitals in Nguigmi, Chetimari and Mainé-Soroa, and several health centres and health posts across the region.
In Mainé-Soroa, we developed cross-border activities to provide access to healthcare for local people and nomadic communities living between Niger and the northernmost fringes of Nigeria’s Yobe state.
Our teams also ran numerous mobile clinics and one-off interventions in areas where the presence of armed groups restricts people’s movements and the delivery of humanitarian assistance.
The mental health needs of children and adolescents traumatised by conflict are often overlooked. We run a mental health and psychosocial programme, through which we have trained 100 community workers to identify symptoms of psychological problems, particularly in young people.
This has vastly increased the number of children we have been able to assist: our teams conducted almost 13,000 individual consultations in 2018, and by the end of the year over 30 per cent of patients were children aged under 14.
Zinder region
Our teams in Zinder region focus on treating children under five for severe acute malnutrition and common childhood diseases.
In 2018, we supported the paediatric unit in Magaria district hospital and 11 health centres, as well as 14 health posts across the region during the seasonal malaria and malnutrition peaks.
We also developed community outreach activities, including awareness raising sessions, active case finding and an initiative training parents to use mid-upper arm circumference (MUAC) measuring tapes to screen their children for malnutrition.
In 2018, we admitted more than 22,000 under-fives to the paediatric unit in Magaria – twice as many as in previous years. We also conducted 127,500 outpatient consultations for children under five and treated 20,900 children in our outpatient feeding programme, almost half of them between August and October.
We reached a point when we admitted more than 1,000 children to hospital in one day, including over 250 children requiring intensive care.
We also assisted the Ministry of Public Health with seasonal malaria chemoprevention activities, carrying out more than 18,000 rapid tests and providing treatment to the 12,200 children who tested positive.
Maradi region
We run another paediatric programme aimed at reducing child mortality in Madarounfa. It comprises inpatient care for severe malnutrition, malaria and other diseases affecting children under five in the district hospital, and outpatient treatment for uncomplicated malnutrition in the surrounding health zones.
From September, we improved active case finding of children with malnutrition by using community health workers to show mothers how to use MUAC tapes.
Through this activity, 253 new cases were identified by the end of the year. MSF-supported community health workers also screened more than 29,800 people for malaria, over 80 per cent of whom tested positive and received treatment.
Due to its proximity to the border, the project receives many patients from Nigeria – they account for up to 30 per cent of malnutrition cases. In early 2018, we started actively searching on both sides of the border for children who had abandoned nutrition treatment prematurely.
Tahoua region
We have been running the inpatient therapeutic feeding centre and paediatric and neonatal units in Madaoua district hospital since 2006. In May 2018, we started supporting outpatient feeding centres and paediatric services in Madaoua and Sabon-Guida health centres.
To reduce maternal mortality, we also had teams working in the maternity ward in Madaoua, and on a sexual and reproductive healthcare programme in Sabon-Guida.
The results of a nutritional and retrospective mortality study we conducted indicated that the situation had stabilised in Madaoua and Sabon-Guida. Based on this and the Ministry of Public Health’s increased capacity, in December we announced our gradual withdrawal from both locations.
Migrants, refugees and host communities
Niger is a major transit country for migrants, asylum seekers and refugees, including people expelled from Algeria, returned from Libya or travelling north towards Europe. These people often face abuse and exclusion.
In 2018, we offered medical care in Niamey and in the region of Agadez, both of which are at the crossroads of migration routes.
Our team in Niamey carried out over 5,000 consultations in fixed and mobile clinics. Across Agadez – in Tabelot, Séguédine, Anaye and Dirkou – we supported primary, reproductive and emergency healthcare and referrals for migrants and local communities.
In Arlit health centre, we provided mental healthcare and organised referrals to Arlit hospital.
In the border village of Assamaka, we provided 1,960 people expelled from Algeria with medical and mental health consultations and distributed relief kits.
In Tillabéri, we reopened inactive primary health centres and ran mobile clinics for local communities and people displaced by interethnic tensions and conflicts in neighbouring Mali and Burkina Faso. We distributed relief kits to 225 families and offered essential medical assistance such as vaccinations, malnutrition screening and reproductive healthcare services.