226,000
226,
15,700
15,7
990
99

9,510
9,51
3,320
3,32
210
21
Life expectancy is steadily increasing in Kenya, with improvements in mortality rates for both HIV and tuberculosis (TB). However, infectious diseases and maternal mortality remain serious concerns.
HIV care in Homa Bay
Despite a generally good coverage of antiretroviral (ARV) therapy, many people living with HIV in Homa Bay county continue to experience treatment failure, and many present at our facilities with advanced HIV co-infections such as Kaposi’s sarcoma. In 2018, we focused on treatment failure, advanced HIV and programmes for adolescents.
More than half the patients admitted to Homa Bay county referral hospital – where MSF supports two adult wards and a tuberculosis (TB) ward – are HIV positive. An average of 18 HIV positive patients died each month in 2018, almost 30 per cent of them within the first 24 hours of admission.
In response, we have implemented various innovative systems, including a dedicated laboratory and point-of-care testing for inpatients, which have facilitated faster treatment. We also run a follow-up clinic at the hospital that liaises with patients' local health facilities to create a continuum of care as close to home as possible.
Providing vital obstetric care in Mombasa
After more than two years of running sexual and reproductive health services from a temporary shipping-container facility in Likoni, Mombasa county, we completed the rehabilitation of Mrima health centre, which opened in May.
The new 36-bed facility has more spacious consultation rooms and upgraded medical equipment, enabling us to provide better care for a higher number of expectant mothers in a densely populated area with no other emergency obstetric or neonatal care facilities.
In 2018, our teams assisted almost 7,000 deliveries, over half of them in the new facility. We also offered antenatal services, medical assistance for victims of sexual violence and health promotion in the community.
Treating non-communicable diseases (NCDs) in Embu
We mentor Ministry of Health staff in Embu county to improve the management of NCDs in primary healthcare facilities. The first cohort of four clinical officers, five nurses and six community health volunteers graduated from the programme in November, having successfully completed modules on asthma, diabetes, hypertension and epilepsy.
Medical care for people who use drugs in Kiambu
Following an assessment in 2018, we noted a significant need for integrated medical care for people who use drugs in Kiambu county. In collaboration with local partners, we carried out an awareness-raising campaign to help the community understand the problem and will open a specialised clinic in Karuri in 2019. Our aim is to reduce the rates of illness and mortality associated with illicit opioid drug use by increasing access to appropriate health services, including different models of opioid substitution therapy and patient support.

Assisting victims of violence in Nairobi
We run an ambulance referral service, a toll-free call centre and a trauma room in Nairobi’s Eastlands area, to improve access to emergency care for victims of urban violence. In 2018, our teams received over 7,600 calls, resulting in 6,230 ambulance interventions and 4,340 referrals to health facilities. The team in the trauma room conducted 9,250 consultations, receiving mostly walk-in patients.
We also run a specialised clinic for victims of sexual and gender-based violence in Eastlands, and support four other facilities run by the Ministry of Health. In 2018, we treated an average of 269 patients a month, representing an 18 per cent increase on the previous year. Our outreach teams increased their community awareness-raising activities, explaining what sexual and gender-based violence is and what assistance is available.
In addition, we continued to support the Ministry of Health in the management of drug-resistant TB (DR-TB), by providing equipment and training. Our ground-breaking DR-TB programme, which we handed over in 2017, introduced the use of GeneXpert machines for diagnosis and oral drugs bedaquiline and delamanid for treatment. We also achieved the country’s first successful treatment of a patient with extensively drug-resistant TB. In 2018, we piloted a nine-month treatment regimen which the Ministry of Health adopted.
Medical care in Dadaab refugee complex
We continue to offer comprehensive healthcare to over 70,000 refugees living in Dagahaley camp in Dadaab and the local community through a 100-bed hospital and two decentralised health posts. In 2018, we conducted more than 175,000 outpatient consultations and admitted over 10,000 patients for care.
Our teams provide a wide range of services, including nutrition support, sexual and reproductive healthcare, emergency surgery, medical and psychological assistance to victims of sexual violence, vaccinations, mental health services, treatment for HIV and TB, palliative care for patients with chronic illnesses and home-based insulin management for people with diabetes.
Emergency responses
Our emergency teams responded to several disease outbreaks and other emergencies in 2018, including ambulance support, medical care and the distribution of relief kits to communities whose homes were ravaged by fires around the country.
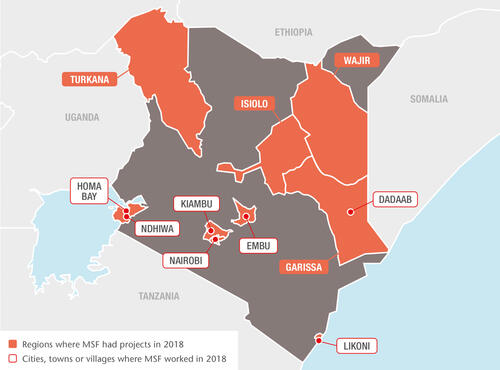
Heavy rains early in the year resulted in a five-month cholera outbreak in Nairobi, Embu, Isiolo, Garissa and Turkana counties. We assisted in the treatment of patients and provided logistical and medical supplies to support the wider response.
In March, we sent staff and medical supplies to support the response to an influenza outbreak in Nanyuki, Laikipia county, and in June, we assisted the Ministry of Health to respond to an outbreak of Rift Valley fever in Wajir county. Caused by a virus transmitted by mosquitoes and blood-feeding flies, Rift Valley fever can lead to potentially lethal haemorrhagic fever. We helped to treat 82 patients and contain the outbreak within a couple of weeks.
At the end of the year, we responded to an influx of wounded patients arriving from the Ethiopian county of Moyale, where violence had erupted. The team supported Takaba district hospital in Mandera county, which received more than 100 wounded within three days.